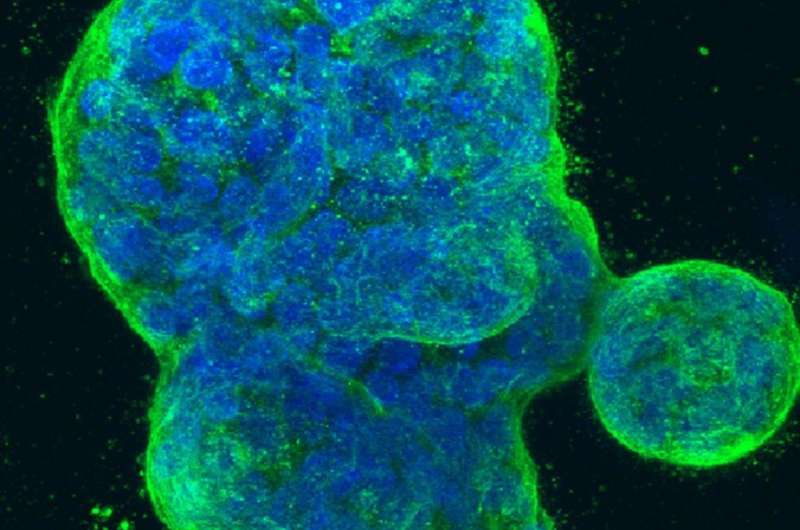
Three-dimensional culture of human breast cancer cells, with DNA stained blue and a protein in the cell surface membrane stained green. Image created in 2014 by Tom Misteli, Ph.D., and Karen Meaburn, Ph.D. at the NIH IRP.
A new editorial explores the wide array of reasons why women who migrate to a new country are less like to attend screening for breast cancer than women born in that country.
Health providers should 'broaden their understanding' of the range of experiences of women in order to increase breast cancer screening uptake, according to a new editorial.
Published in the British Medical Journal and written by Dr. Elizabeth Davies and Yueh-Hsin Wang, the article describes how providers need to look beyond existing measures and consider the complex nature of barriers facing women who have migrated to another country.
It's established that attendance for breast cancer screening is lower among migrants than in women born in high income countries. Previous research has emphasized the impact of language barriers in contributing to these disparities.
However, Dr. Davies and Wang explain how a major randomized controlled trial found that translated invitations didn't have a significant effect on screening uptake in Norway. Considering these results, the editorial argues that we must 'broaden our understanding' of the experience of migrating as a woman to look beyond language barriers.
Women who have migrated to a new country will also encounter additional administrative barriers in attending health appointments, as well as bring differing perceptions of breast cancer risk and varying levels of trust in official health care systems.
Australia has one of the highest proportion of migrants among major high-income countries and has sought to minimize health inequalities among migrant groups, particularly refugees and asylum seekers. Research interviews suggest that the approach and sex of general practitioners or family doctors, women's awareness and knowledge of cancer screening, financial problems, and language difficulties all contribute to attendance for cancer screening.
Alongside this, the authors note how UK-based studies found that women of Caribbean, African and Bangladeshi descent were less likely to attend breast screening than women from white ethnic backgrounds. However, uptake was found to have increased in Bangladeshi women when screening initiatives were led by Bangladeshi GPs.
When reviewing these recent insights, the authors argue that local health services and policy makers should look to develop "more nuanced, multifaceted, and targeted interventions" to help engage women who do not attend for screening. This can only be achieved with an understanding of the many challenges women may face when migrating to a new country.
"One element may be for services to reconsider how long they label women as 'immigrant' rather than viewing them as settled citizens from diverse cultural backgrounds," says Dr. Elizabeth Davies, Clinical Reader in Cancer and Public Health.
More information: Elizabeth A Davies et al, Understanding inequalities in breast cancer screening uptake, British Medical Journal (2023). DOI: 10.1136/bmj.p2084
Journal information: British Medical Journal (BMJ)
Provided by King's College London