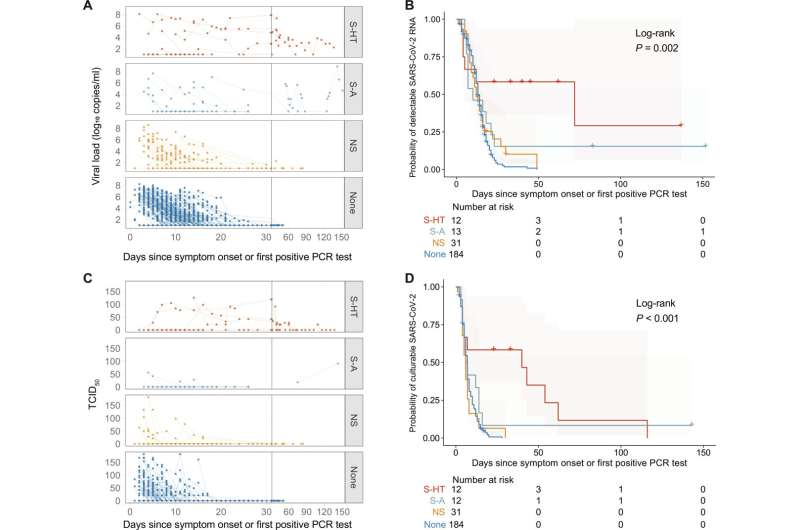
Kinetics of SARS-CoV-2 viral RNA and culturable virus varied among the immunocompromised groups. (A) Upper respiratory viral RNA decay is shown. The lower level of quantification (LLOQ) is 10 copies/ml. (B) Kaplan-Meier estimates of upper respiratory viral clearance are shown (viral load below LLOQ), and global log-rank P values were shown. For (A) and (B), n = 12, 13, 31, and 184 for S-HT, S-A, NS, and nonimmunocompromised groups, respectively. (C) Upper respiratory culturable virus dynamics were quantified as TCID50 values. (D) Kaplan-Meier estimates of upper respiratory culturable virus clearance were shown, and global log-rank P values were shown. For (C) and (D), n = 12, 12, 31, and 184 for S-HT, S-A, NS, and nonimmunocompromised groups, respectively. Credit: Science Translational Medicine (2024). DOI: 10.1126/scitranslmed.adk1599
Individuals who are immunocompromised are at risk of worse COVID-19 outcomes and may have a less robust response to vaccination compared to non-immunocompromised individuals. But the term "immunocompromised" refers to a wide range of conditions, and not all patients in this category may be at equal risk.
Researchers from Mass General Brigham have studied a population of 56 immunocompromised individuals that included patients who were severely immunocompromised due to hematologic malignancies/organ transplant or auto-immune/B cell deficiency as well as non-severely immunocompromised patients. The team compared these groups to one another and to patients who were not immunocompromised.
They found that patients' abilities to clear the virus differed by the extent of their immunosuppression. Patients who were immunocompromised due to a hematologic malignancy or organ transplant were most likely to have a chronic, prolonged infection. This finding suggests the importance of T cells in clearing SARS-CoV-2 infection, which has implications for patient monitoring and improved vaccine design. Participants who were severely immunocompromised also had a higher risk of developing resistance against therapeutic monoclonal antibodies.
The study is published in the journal Science Translational Medicine.
"Providers and patients should be aware that protracted symptoms may mean persistent COVID-19 disease that requires additional testing and potential treatment," said corresponding author Jonathan Li, MD, of the Division of Infectious Diseases at Brigham and Women's Hospital.
Patients with a history of organ transplant or hematologic malignancy had the greatest delay in viral clearance; patients with B cell immunodeficiency had an intermediary risk; and the study's 31 patients with mild, non-severe immunocompromise, such as those with autoimmune diseases receiving anti-tumor necrosis factor (TNF) treatment, had similar viral shedding dynamics to non-immunocompromised participants.
"While our sample size is limited, these results provide reassurance that most patients with mild/moderate immunosuppression (including those on B-cell depleting therapy) will be able to clear the virus during the acute phase of infection," said Li.
More information: Yijia Li et al, SARS-CoV-2 viral clearance and evolution varies by type and severity of immunodeficiency, Science Translational Medicine (2024). DOI: 10.1126/scitranslmed.adk1599
Journal information: Science Translational Medicine
Provided by Mass General Brigham