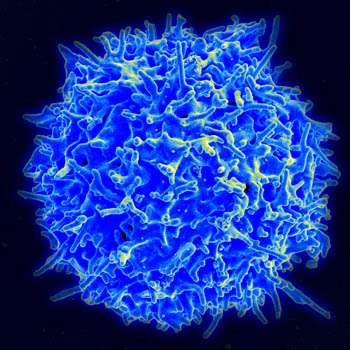
Scanning electron micrograph of human T lymphocyte or T cell. Credit: NIAID/NIH
Higher or lower levels of certain immune cells in cancer patients may be associated with how well they respond to immunotherapy, according to preliminary results of a study conducted by researchers at the University of Pittsburgh Cancer Institute (UPCI).
The findings will be presented today at the American Association of Cancer Research (AACR) Annual Meeting in Washington, D.C., by Robert Ferris, M.D., Ph.D., UPMC Endowed Professor, chief of the Division of Head and Neck Surgery, and co-leader of the Cancer Immunology Program at UPCI.
The research was an extension of the recently completed CheckMate 141 Phase III clinical trial co-chaired by Dr. Ferris, which showed that the immunotherapy nivolumab significantly increases survival and causes fewer adverse side effects in patients with recurrent head and neck cancer.
However, the treatment was not equally effective in all the patients so Dr. Ferris and his team aimed to find out whether differences in the patients' immune system profiles could be associated with better response to immunotherapy.
The researchers found that higher levels of tumor-associated immune cells (TAICs) expressing the PD-L1 protein were associated with longer overall survival and greater likelihood of response to the drug nivolumab. TAICs are immune cells that have infiltrated the tumor and are thought to play an important role in tumor growth.
In blood samples taken prior to the start of immunotherapy, the researchers also found that patients with higher levels of circulating CD8, or cytotoxic, T cells—also known as killer T cells—and lower levels of regulatory T cells were associated with better response to treatment.
"Our study shows that immune cells in the microenvironment around the tumor could play a critical role in how patients respond to immunotherapy. By determining the nature of these cells and how they are affected by treatments, we may be able to significantly improve the effectiveness of current therapies and help a greater number of patients," said Dr. Ferris.
More information: This study was funded by UPCI and Bristol-Myers Squibb.