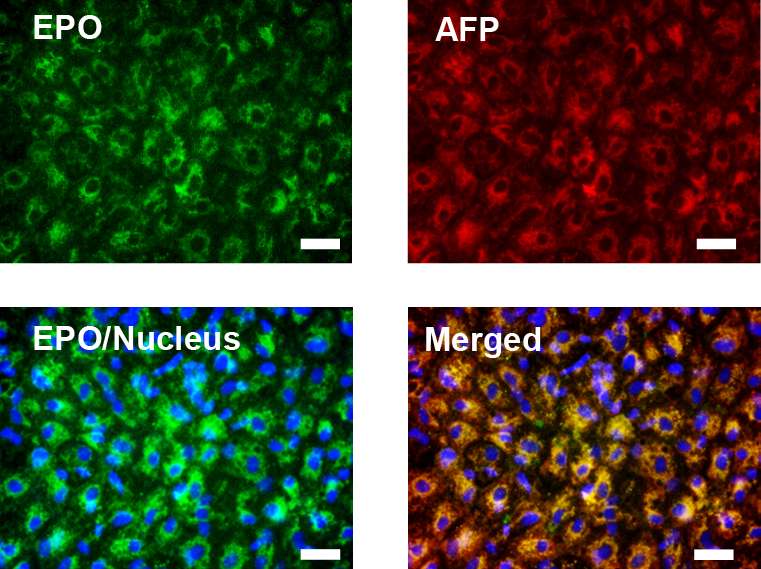
Microscopic images of stem-cell derived EPO-producing cells that were used to treat renal anemia in mice. Credit: H. Hitomi et al., Science Translational Medicine (2017)
(Medical Xpress)—A team of researchers with Kyoto University and Kagawa University, both in Japan, has cured renal anemia in mice by injecting them with treated human stem cells. In their paper published in Science Translational Medicine, the group describes their approach and how well it worked.
Chronic kidney disease is a serious ailment resulting in a host of symptoms due to the body's reduced ability to process waste and fluids—many patients eventually experience renal failure, which requires them to undergo routine dialysis or a kidney transplant. Less well known is that people with chronic kidney disease also suffer from renal anemia because the kidneys manufacture the hormone erythropoietin (EPO), which causes the body to produce red blood cells without which the blood cannot carry enough oxygen to the brain and other body parts. The current treatment for renal anemia is injections of EPO every few days, which, for many people, is impractical because of the cost and side effects. In this new effort, the researchers have found a possible new treatment—injecting treated stem cells directly into the kidneys.
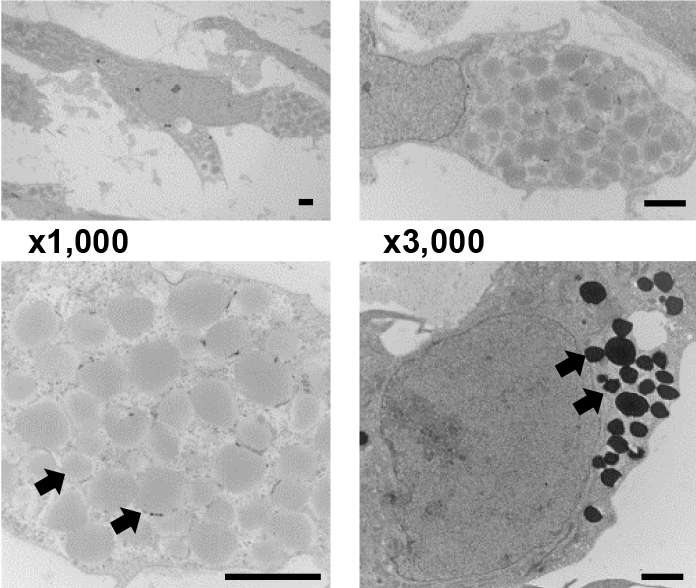
In their experiments, the researchers collected stem cells from human cord blood (from the umbilical cord) and then treated them with growth factors that changed them to pluripotent stem cells that grew into mature cells capable of producing EPO. The team then injected the treated cells into the kidneys of mice suffering from renal anemia and monitored them for the rest of their lives.
Progressively zoomed-in images of stem-cell derived EPO-producing cells and mouse liver for comparison (bottom right), showing secretory structures called vesicles (indicated by arrows). Credit: H. Hitomi et al., Science Translational Medicine (2017)
The team reports that for all of the mice tested, EPO levels were approximately 20 times higher than for control mice after just four weeks—putting them in the normal range. They report also that the levels were maintained through the life of the mice, which, the team notes, means they were cured of the ailment.
It is not clear yet, of course, whether the procedure would work with human patients, but the group intends to continue their research with the goal of finding out. If the procedure works as intended and does not cause harmful side effects, people in the future suffering from kidney disease may no longer have to worry about also dealing with anemia.
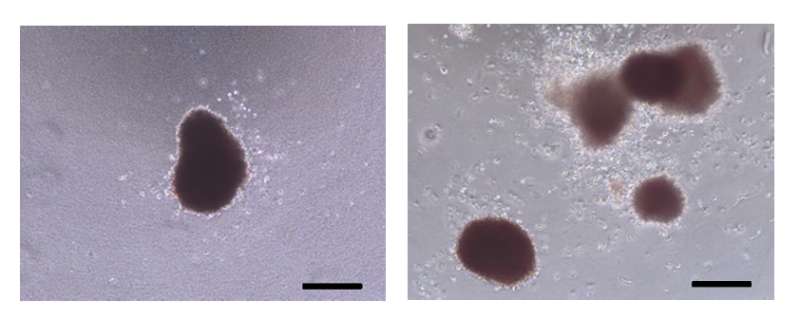
Images of blood cells forming in response to purified EPO protein from conventional sources (left) and from stem-cell derived EPO producing cells (left). Credit: H. Hitomi et al., Science Translational Medicine (2017)
More information: Hirofumi Hitomi et al. Human pluripotent stem cell–derived erythropoietin-producing cells ameliorate renal anemia in mice, Science Translational Medicine (2017). DOI: 10.1126/scitranslmed.aaj2300
Abstract
The production of erythropoietin (EPO) by the kidneys, a principal hormone for the hematopoietic system, is reduced in patients with chronic kidney disease (CKD), eventually resulting in severe anemia. Although recombinant human EPO treatment improves anemia in patients with CKD, returning to full red blood cell production without fluctuations does not always occur. We established a method to generate EPO-producing cells from human induced pluripotent stem cells (hiPSCs) by modifying previously reported hepatic differentiation protocols. These cells showed increased EPO expression and secretion in response to low oxygen conditions, prolyl hydroxylase domain–containing enzyme inhibitors, and insulin-like growth factor 1. The EPO protein secreted from hiPSC-derived EPO-producing (hiPSC-EPO) cells induced the erythropoietic differentiation of human umbilical cord blood progenitor cells in vitro. Furthermore, transplantation of hiPSC-EPO cells into mice with CKD induced by adenine treatment improved renal anemia. Thus, hiPSC-EPO cells may be a useful tool for clarifying the mechanisms of EPO production and may be useful as a therapeutic strategy for treating renal anemia.
Journal information: Science Translational Medicine
© 2017 Medical Xpress