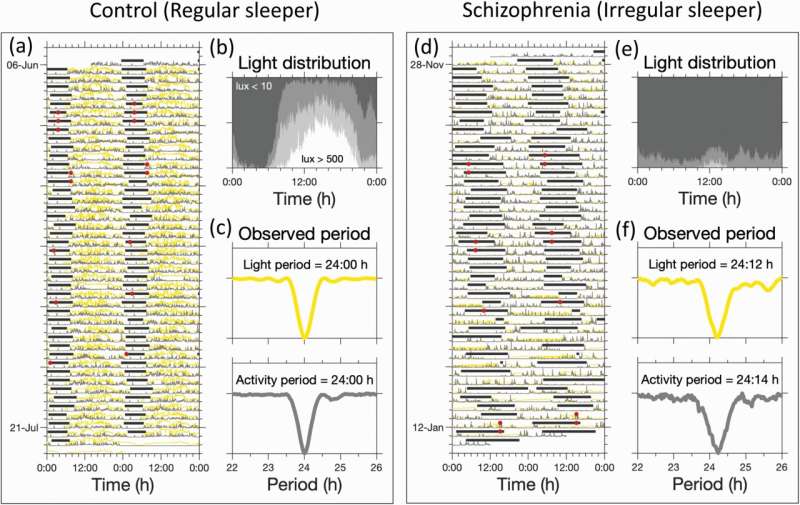
Typical rhythms of sleep, activity and light exposure. (a), (d): Light (yellow trace), activity (gray trace), 6-sulphatoxymelatonin (aMT6s) acrophase (red circles) and sleep timing (horizontal gray bars). (b) and (e): Average pattern of light exposure across the 24-h day. The shaded regions from white through to dark gray indicate the fraction of time spent at different light levels (>500 lux; between 500 and 100 lux; between 100 and 10 lux, <10 lux). (c) and (f) Residual variance as a function of period for activity and light. These indicated that light and activity followed a 24 h pattern for the regular sleeper, but a longer than 24-h pattern for the irregular sleeper. Credit: DOI: 10.1093/schbul/sbab124
Disturbed sleep timing in people living with schizophrenia is more likely to be related to light exposure than to intrinsic biological factors.
Application of a physiologically-based mathematical model to light exposure, sleep timing data and biological markers of the circadian clock, has revealed that disturbed sleep timing in people living with schizophrenia is more likely to be related to light exposure than to intrinsic biological factors. Surprisingly, the combination of the mathematical model and digital health data suggested that normalization of disturbed sleep timing can be achieved by improving light availability and does not require the imposition of altered sleep timing or sitting in front of light boxes as recommended in current bright light intervention therapies.
It is well known that sleep timing is altered in people living with mental health conditions, including those living with schizophrenia, and contributes to poor sleep. Poor sleep is often associated with distress, worse mental health and poorer quality of life. Consistent with other studies, the current reanalysis of previously published data found that people living with schizophrenia spend more time in bed, wake up later and sleep in a more irregular pattern. In some participants sleep drifted through the 24-hour day, particularly in the winter months.
Whether altered sleep timing patterns are related to changes in biologically-determined characteristics of the body clock that drives sleep timing, or to behaviourally determined patterns of light exposure which normally synchronize the clock to the 24-hour day, is an active topic of debate.
The multidisciplinary team of a mathematician, circadian and sleep physiologists and a psychiatrist at the University of Surrey, the University of Umeå (Sweden) and King's College London respectively joined forces to address this issue. Feeding the unique data through a mathematical model which includes the biological factors that underlie sleep timing and how the body clock is affected by environmental factors revealed that light exposure is the main determinant.
Although the importance of light has previously been recognized, current interventions require people to sit in front of light boxes that give out bright light at specific times of the day. These interventions stipulate that for maximum benefit people living with schizophrenia need to force themselves to wake up and sleep on a fixed schedule. The mathematical analyses demonstrate that this is not necessary. The much more easily implemented solution is to change the light availability pattern and the mathematical principles of how sleep timing is regulated by light will do the rest.
Importantly, this approach can be geared to individual differences and can be implemented by using currently available digital health technology. Such interventions could be co-designed with patients, making them easier to stick to. By increasing adherence and tuning them to individuals, light interventions could become a more effective method to address sleep disturbances.
In their paper, the authors describe a pathway for implementation of their approach which could become a template for how data-model fusion techniques may help reduce sleep disturbance in a wide range of disorders including schizophrenia, bipolar disorders, delayed sleep phase syndrome and dementia. Dementia is the current focus of the Surrey researchers as a result offundingfrom theUK Dementia Research Institute.
Professor Anne Skeldon from the University of Surrey'sDepartment of Mathematics said:
"Our clinical framework suggests a cost-effective way to help people sleep at more regular times through 'light availability' interventions that are co-designed with individuals to fit into their daily lives. With guidance from clinicians, a wearable device to measure light and appropriate software, light interventions could take into account individual physiological characteristics and preferences."
Professor Derk-Jan Dijk from the Surrey Sleep Research Centre said:
"Combining digital health technology to collect data with mathematical models for the effects of light on circadian rhythms and sleep timing is a powerful approach to develop personalized interventions."
Associate Professor Katharina Wulff from Umeå University in Sweden said:
"With these technologies at hand, the response to the strong seasonal daylight changes up here in the Northern part of Sweden could potentially be tracked by individuals and processed by mathematical modeling for personalized light regimes when supplementary light is required."
More information: Anne C Skeldon et al, Extracting Circadian and Sleep Parameters from Longitudinal Data in Schizophrenia for the Design of Pragmatic Light Interventions, Schizophrenia Bulletin (2021). DOI: 10.1093/schbul/sbab124
Provided by University of Surrey