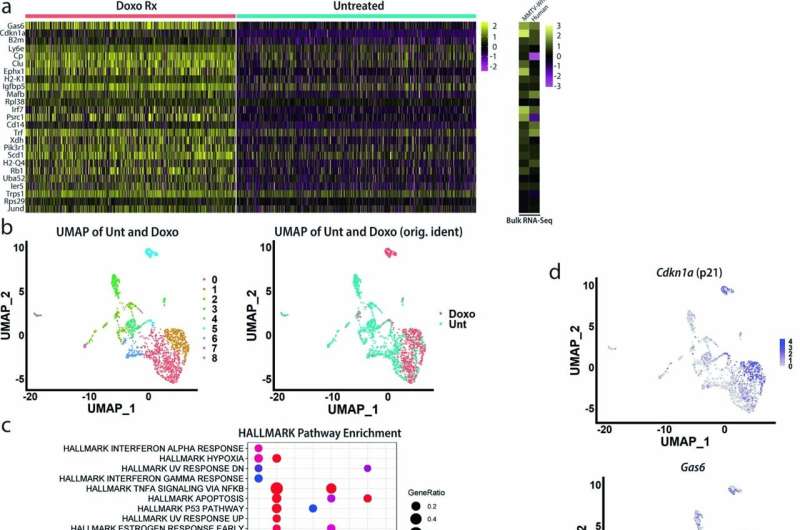
10X Genomics scRNA-seq was performed on MMTV-Wnt1 mammary tumor transplants from doxorubicin treated and untreated mice. Sequenced cells from untreated and treated tumors were pooled, standard quality control and data processing performed, and clusters and cells with reads for Ptprc (CD45) were removed to deplete immune cells. a) Heat map depicting the top 25 upregulated genes between the doxorubicin treated and untreated cells (elements represented in heatmaps are normalized average log2 counts). b) UMAP dimensional reduction analysis was performed, revealing nine distinct clusters (left); original identities of cells (Doxo or Unt) are shown on right. c) Dot plot was generated showing enriched HALLMARK pathways using the top 100 upregulated genes in each cluster. P-values for upregulated genes were determined using a Wilcoxon Rank Sum test. d) Feature plots depicting expression levels of indicated genes were generated. e) Feature plots depicting enrichment of indicated genesets/signatures were generated. Credit: Nature Cancer (2022). DOI: 10.1038/s43018-022-00466-y
Thanks to advances in cancer therapies, most forms of breast cancer are highly treatable, especially when caught early.
But the last frontier cases—those that can't be treated with hormone or targeted therapies and don't respond to chemotherapy—remain the deadliest and hardest to treat. Tulane University researchers have discovered for the first time how these cancers persist after chemo and why they don't respond well to immunotherapies designed to clear out remaining tumor cells by revving up the immune system.
The process of surviving chemotherapy triggers a program of immune checkpoints that shield breast cancer cells from different lines of attack by the immune system. It creates a "whack-a-mole" problem for immunotherapy drugs called checkpoint inhibitors that may kill tumor cells expressing one checkpoint but not others that have multiple checkpoints, according to a new study published in the journal Nature Cancer.
"Breast cancers don't respond well to immune checkpoint inhibitors, but it has never really been understood why," said corresponding author James Jackson, Ph.D., associate professor of biochemistry and molecular biology at Tulane University School of Medicine. "We found that they avoid immune clearance by expressing a complex, redundant program of checkpoint genes and immune modulatory genes. The tumor completely changes after chemotherapy treatment into this thing that is essentially built to block the immune system."
Researchers studied the process in mouse and human breast tumors and identified 16 immune checkpoint genes that encode proteins designed to inactivate cancer-killing T-cells.
"We're among the first to actually study the tumor that survives post-chemotherapy, which is called the residual disease, to see what kind of immunotherapy targets are expressed," said the study's first author Ashkan Shahbandi, an MD/Ph.D. student in Jackson's lab.
The tumors that respond the worst to chemotherapy enter a state of dormancy—called cellular senescence—instead of dying after treatment. Researchers found two major populations of senescent tumor cells, each expressing different immune checkpoints activated by specific signaling pathways. They showed the expression of immune evasion programs in tumor cells required both chemotherapy to induce a senescent state and signals from non-tumor cells.
They tested a combination of drugs aimed at these different immune checkpoints. While response could be improved, these strategies failed to fully eradicate the majority of tumors.
"Our findings reveal the challenge of eliminating residual disease populated by senescent cells that activate complex immune inhibitory programs," Jackson said. "Breast cancer patients will need rational, personalized strategies that target the specific checkpoints induced by the chemotherapy treatment."
More information: Breast cancer cells survive chemotherapy by activating targetable immune-modulatory programs characterized by PD-L1 or CD80, Nature Cancer (2022). DOI: 10.1038/s43018-022-00466-y
Journal information: Nature Cancer
Provided by Tulane University