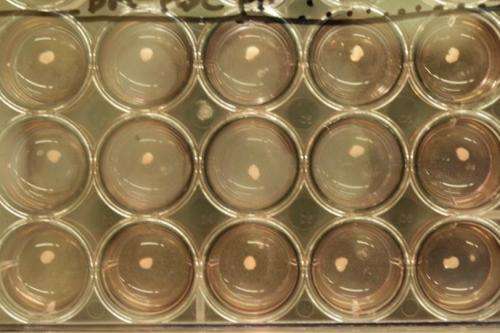
Human iPSC-derived liver bud. Credit: Takanori Takebe
Scientists in Japan said Wednesday they had grown human liver tissue from stem cells in a first that holds promise for alleviating the critical shortage of donor organs.
Creating lab-grown tissue to replenish organs damaged by accident or disease is a Holy Grail for the pioneering field of research into the premature cells known as stem cells.
Now Takanori Takebe of the Yokohama City University Graduate School of Medicine and a team report in the journal Nature that they grew tissue "resembling the (human) adult liver" in a lab mouse.
They first created induced pluripotent stem (iPS) cells which they mixed with other cell types and coaxed into "liver buds"—the precursor clusters that develop into a liver.
The buds, each about five millimetres (0.2 inches) big, were then transplanted onto a mouse brain, where they were observed transforming into a "functional human liver" complete with blood vessels, the scientists wrote.
"To our knowledge, this is the first report demonstrating the generation of a functional human organ from pluripotent stem cells," said the report.
The technique has yet to be tested in humans, but serves as an important proof of concept, it added.
Stem cells are infant cells that can develop into any part of the body.
Until a few years ago, when iPS cells were created, the only way to obtain stem cells was to harvest them from human embryos.
Liver bud formation process from human iPSC. This video shows formation of human induced pluripotent stem cell-derived liver bud by recapitulating organogenetic interactions. After mixing three-cell types at particular timing, we seeded cells onto the dish to start liver bud formation. This is a 72hour timelapse movie for liver bud forming process at the beginning of mixed cell seeding. Credit: Takanori Takebe
This is controversial because it requires the destruction of the embryo, a process to which religious conservatives and others object.
iPS cells are easily-obtainable mature cells that are "reprogrammed" into a versatile, primitive state from where they can develop into any kind of cell in the body.
Takebe told a press conference ahead of the report's release that the man-made liver was observed through a replacement glass skull that was fitted around the mouse's brain.
The liver developed blood vessels which fused with those of the animal.
It also performed certain human-specific liver functions—producing proteins and processing specific drugs.
"We have concluded that this liver is functioning," the scientist said. "We think this is enough for improving the survival after liver failure."
Scientists commenting on the research described it as promising.
"This science opens up the distinct possibility of being able to create mini-livers from the skin cells of a patient dying of liver failure," said Malcolm Alison, professor of stem cell biology at the Queen Mary University of London.
"Human mature liver cells transplanted on their own can fail to thrive, but if immature liver cells are first combined with their normally nurturing supportive cells, they can mature in the transplanted host and function efficiently," he said in a statement issued by the Science Media Centre.
Dusko Ilic from Kings College London said "the promise of an off-shelf-liver seems much closer than one could hope even a year ago", but the strategy has yet to be proven in humans.
"Whilst the title of the paper is 'functional human liver', these liver buds do not contain the biliary structures (which drain toxins out of the liver) or immune cells that characterise real human liver," added Stuart Forbes, professor of transplantation and regenerative medicine at the University of Edinburgh.
Chris Mason of University College London said the buds may be useful for drug testing in the lab, which is currently restricted by the limited availability of liver cells from human cadavers.
Takebe said the method may also work in organs like the pancreas, kidneys or lungs, but it would be another 10 years before trials are done in humans.
One key requirement would be to shrink the "buds" to a much smaller size so they can be injected into the bloodstream and taken up by the body internally, he said.
More information: Paper: dx.doi.org/10.1038/nature12271
Journal information: Nature
© 2013 AFP