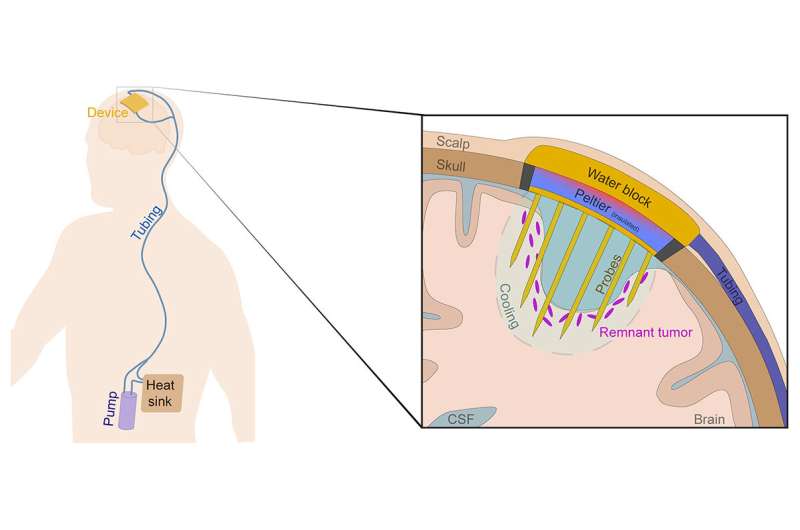
Conceptual model of a translational device to deliver cytostatic hypothermia for GBM. Representative diagram of a patient with GBM implanted with an envisioned cytostatic hypothermia system with zoomed inset of device (right). The envisioned system consists of an intracranial device consisting of a multiprobe array in conjunction with a cooling Peltier plate and a water block. An implanted, nonlocal, nonmagnetic pump facilitates water flow through tunneled, subcutaneous tubing to carry heat away from the hot side of the Peltier plate and distribute it to the surrounding skin via the tubing and a subcutaneous heat sink. Inset shows a slice of the cranial cavity after tumor resection with a hypothetical cytostatic hypothermia device and the remaining nonresectable tumor cells. A multiprobe array is envisioned to facilitate homogeneous cooling at the site of possible tumor recurrence. Credit: Science Advances (2022). DOI: 10.1126/sciadv.abq4882
A new preclinical study recently reported in Science Advances, led by researchers currently at Emory and UT Southwestern (UTSW) who began it while they were at Duke University, suggests that cooling brain tumors to room temperature may extend survival of patients with glioblastoma multiforme (GBM).
Glioblastoma multiforme (GBM) persists as a form of cancer with a grim prognosis. Despite standard-of-care treatment, patients with this type of brain tumor have a poor median survival of 15 to 18 months. On average, fewer than 7% survive five years after diagnosis. The prognosis is challenging because even the most effective therapies currently available are not able to prevent GBM from recurring.
Joining the growing list of potential, novel therapies—such as manipulating electric fields and temperature—is a revived concept first tried in the 1940s with early attempts at cryogenic freezing of brain tumors. Although freezing tumors could remove diseased tissue, the sub-zero temperatures also harmed healthy tissue around it.
But a study led by authors Syed Faaiz Enam, MBBS, Ph.D., of UT Southwestern, and Ravi V. Bellamkonda, Ph.D., of Emory University, finds that "cytostatic hypothermia," which locally and continuously cools the brain tumor without harming surrounding healthy tissue, is able to prolong the survival of rats with brain tumors.
Enam is currently a neurology resident and scientist at the University of Texas Southwestern Medical Center and previously a postdoctoral researcher at Duke University's Pratt School of Engineering. Bellamkonda is currently provost and executive vice president for academic affairs at Emory and a researcher at Winship Cancer Institute of Emory University. He came to Emory in 2021 from Duke University, where he was dean of the Pratt School of Engineering.
The research team created and implanted hypothermia devices onto rats who were still able to eat, grow and move around freely. Those that had their device switched on—that is, had their brain tumors cooled to room temperature—survived at least twice as long. Promisingly, those rats whose tumors reached their "cytostatic" temperature—that is the temperature at which the tumor stops growing—survived the full study period.
Bellamkonda explains that this work demonstrates that tumor cells stop growing at room temperature, 68-77 degrees Fahrenheit, compared to the normal body temperature of 98.6 degrees. Hypothermia (cooling) seems to slow multiple cell processes, which might be why tumors stop growing; this may also prevent the development of resistance to chemotherapy or immunotherapy, a significant problem in the cancer space.
The next step in the ongoing research will be to design a prototype for a larger-size device and try it on other animals and humans.
Enam is confident it can work. "Since temperature is a fundamental physical property, and all chemical and cellular reactions depend on it," he says, "the effects would be matched in other tumor types and other species as well." He adds, "Results are not limited to rats. It should work for humans too. It is fundamental physics that affects biology broadly."
The authors envision several potential outcomes of the research: A patient might have the device permanently implanted "and it keeps the remaining tumor cells at bay." Or they "may only need the device for a certain period of time because tumors might be selectively sensitive to prolonged hypothermia." A third possibility might be using the device in conjunction with chemotherapies or immunotherapies—as the research article discusses. In this case, Bellamkonda says, "hypothermia would keep the remaining tumor cells at bay so they don't evolve resistance."
Cytostatic hypothermia may prove to be a powerful weapon against GBM, one of the most lethal forms of cancer—and other tumors as well.
"In a manner, this is a new field," says Enam. "We've tried many different ways to kill cancer. However, when we do, it comes back stronger, it evolves. This is a rethink of our approach to cancer. Instead of killing it, we are stopping its growth. This buys time to try different therapies until we find a cure for any particular patient."
More information: Syed Faaiz Enam et al, Cytostatic hypothermia and its impact on glioblastoma and survival, Science Advances (2022). DOI: 10.1126/sciadv.abq4882
Journal information: Science Advances
Provided by Emory University