Graphical abstract. Credit: Bioactive Materials (2023). DOI: 10.1016/j.bioactmat.2023.05.015
Myocardial infarction (MI) and the resulting heart failure remain a leading cause of morbidity and mortality worldwide. Cell therapy by implantation of stem/progenitor cells and their derived cardiovascular cells offers new opportunities to repair infarcted hearts.
Prof. Yang Huangtian's team from Shanghai Institute of Nutrition and Health of the Chinese Academy of Sciences and other laboratories have demonstrated the beneficial effects of implantation of human pluripotent stem cell-derived cardiovascular progenitor cells (hCVPCs) and human cardiomyocytes (hCMs) into infarcted hearts in murine, porcine, and non-human primate models of MI, but low engraftment of hCVPCs and incidence of ventricular arrhythmias following intramyocardial injection of hCMs are observed. More research is needed to determine suitable cell types, mechanisms underlying, and optimal approaches to enhance the therapeutic efficacy and safety of cell therapy.
The intact porcine small intestinal submucosa (SIS) extracellular matrix (ECM) materials have a superior biocompatibility to support stem cell attachment and growth and promote angiogenesis and cardiac function after implantation in MI hearts. However, it is not known whether it can be used to construct hPSC-derived cardiovascular cell patches and whether these cell-seeding SIS patches can promote the repair of infarcted hearts better than the SIS-ECM alone.
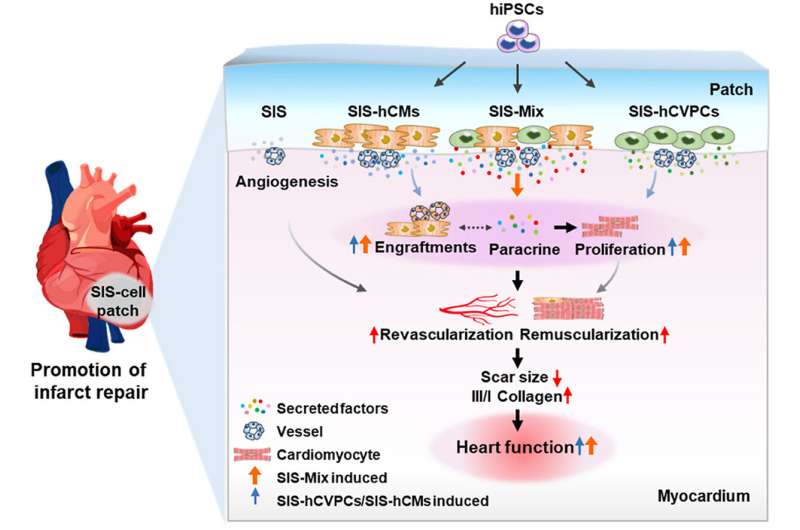
In a study published in Bioactive Materials, Prof. Yang's team and the collaborators developed a strategy to promote cardiac repair with engineered mono- and dual-human pluripotent stem cells (hPSCs)-derived cardiovascular progenitors (hCVPCs)- and cardiomyocytes (hCMs)-seeding ECM patches. The cell-seeding patches display long-term functional improvements, smaller scar and reversed maladaptive remodeling in the infarcted hearts after being epicardially implanted at the sub-acute phase of MI, and the dual cell-seeding patches show better therapeutic effects.
The researchers did a side-by-side comparison of epicardial implantation of the SIS patches alone and the SIS-seeded mono-hCVPC-, hCM-, and dual hCVPC + hCM (Mix) patches at seven days post-MI in a mouse model for cardiac repair. They found that the SIS patches have good biocompatibility to hCVPCs and hCMs, and they improve cell viability. They also discovered that epicardial implantation of mono- and dual-cell seeding SIS patches significantly preserves cardiac function and decreases scar formation at day 28, and is concomitantly associated with increased vascularization and cardiomyocyte proliferation. The same results are not seen with the SIS alone.
In addition, the researchers discovered that the SIS-Mix patches have better therapeutic effects characterized by more effective short- and long-term improvements of left ventricular performance and dilation, and show an enhancement of engraftment and cardiomyocyte proliferation. Proteomic analysis showed distinct biological functions of exclusive proteins secreted from hCVPCs and hCMs, and more exclusive proteins secreted from co-cultivated hCVPCs and hCMs than mono-cells involving in various functional processes essential for infarct repair.
These findings are the first to demonstrate the efficacy and mechanisms of mono- and dual-hCVPC- and hCM-seeding SIS-ECM for repair of infarcted hearts based on the side-by-side comparison. The implantation of dual hCVPC- and hCM-seeding SIS patches exhibits synergistic and complementary effects in promoting infarct repair, which might be a promising therapeutic approach for ischemic heart disease.
More information: Yun Jiang et al, Dual human iPSC-derived cardiac lineage cell-seeding extracellular matrix patches promote regeneration and long-term repair of infarcted hearts, Bioactive Materials (2023). DOI: 10.1016/j.bioactmat.2023.05.015
Provided by Chinese Academy of Sciences