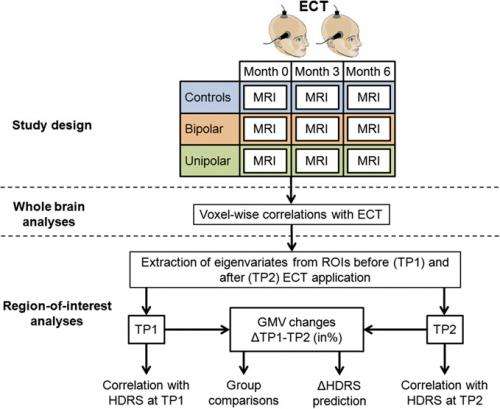
Schematic representation of study design and statistical analyses. ECT given at any time point if clinically indicated. Credit: Copyright © PNAS, doi:10.1073/pnas.1321399111
(Medical Xpress)—The oldest well-established procedure for somatic treatment of unipolar and bipolar disorders, electroconvulsive therapy (ECT) has, at best, a variegated reputation – and not just in its reputation for being a "barbaric" treatment modality (which, as it turns out, it is not). The scientific, clinical, and ethical controversy extends to unanswered questions about its precise mechanism of action – that is, how major electrical discharge over half the brain shows efficacy in recovery from a range of sometimes quite distinct psychological and psychiatric disorders. Recently, however, scientists at Université de Lausanne, Lausanne, Switzerland and Charité University Medicine, Berlin, Germany found local but not general anatomical brain changes following electroconvulsive therapy that are differently distributed in each disease, and are actually the areas believed to be abnormal in each disorder. Since interaction between ECT and specific pathology appears to be therapeutically causal, the researchers state that their results have implications for deep brain stimulation, transcranial magnetic stimulation and other electrically-based brain treatments.
Prof. Bogdan Draganski discussed the paper that he, Dr. Juergen Dukart and their co-authors published in Proceedings of the National Academy of Sciences. The scientists face a number of challenges when conducting their study, the first being using a whole-brain approach to resolve ambiguities in region-of-interest (ROI) imaging studies in ECT treatment of mood disorders. "ROI analyses compress a complex signal pattern into a regional average, thus losing the anatomical specificity of the structural data obtained," Draganski tells Medical Xpress. "Considering the pattern of functional and structural connectivity of the brain, regional changes are frequently associated with alterations in remote areas of the brain which will not be captured in a ROI analysis. Moreover, there are many methodological and technical issues concerning choice of region-of-interest, its spatial extent, inter-individual variability, and so on." At the same time, he adds, whole-brain studies are much more the standard rather than the exception in the field of computational anatomy.
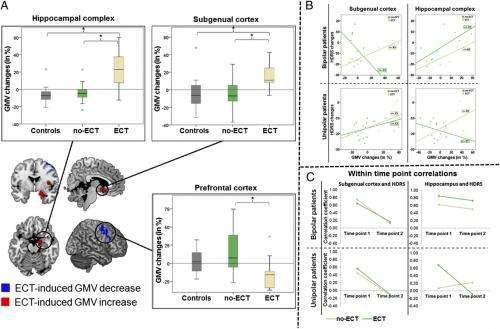
The researchers also had to demonstrate the link between localization of electroconvulsive therapy (ECT)-induced structural brain plasticity and treatment effects. "ECT has been heavily disputed since its introduction," Draganski explains, "and is often described as a 'barbaric' placebo effect. However," he points out, "ECT is the most efficient non-pharmacological treatment in mood disorders – a fact that vanishes in non-scientific discussions and reasoning." Underscoring this point, in a whole-brain approach the scientists demonstrated a specific effect of right unilateral ECT on the brain with ECT-associated grey matter volume increase in hippocampus and subgenual grey – both areas implicated in mood disorders.
"If we consider findings in epilepsy patients with a seizure-related boost in neurogenesis" – the production of new neurons – "in the hippocampus, and the fact that ECT induces an epileptic seizure, the presumption here is that we confirm the notion of increased post-ECT neurogenesis," Draganski says. "The challenge remains how to focus electric currents in a way that they induce similar effects in a set of affected brain regions according to the underlying pathology of a certain brain disorder."
Results of post hoc analyses. (A) Plots of the mean hippocampal, prefrontal, and subgenual GMV, changes (in percent) induced by ECT treatment compared with no-ECT patients and control subjects. (B) Correlation coefficients obtained between changes in subgenual (Left) and hippocampal (Right) GMV, and changes in the HDRS. Results are displayed separately for bipolar and unipolar depression patients subdivided by treatment condition (ECT vs. no-ECT). (C) Correlation coefficients between HDRS scores and subgenual (Left) and hippocampal (Right) GMV and the time point before and after ECT treatment, choosing suitable control periods in no-ECT patients. Results are displayed separately for bipolar (Upper) and unipolar (Lower) depression patients subdivided by treatment condition. An asterisk represents significant difference between the groups at a threshold of P < 0.05 (two-tailed, Bonferroni corrected). Credit: Copyright © PNAS, doi:10.1073/pnas.1321399111
In fact, Draganski continues, up until to now there has been much controversy over exactly how deep brain stimulation and transcranial magnetic stimulation work. "We show that electrical currents applied unilaterally to the brain not only lead to symptom improvement in patients suffering from mood disorders, but also induce specific changes in key brain areas involved either in unipolar depression or bipolar disorder. Research in the field should therefore focus on studying in detail the distribution patterns of electric current fields in the brain, further modulated through intensity changes and duration of application, to answer pertinent questions about the local and remote effects of these electrically-based treatments." Moreover, he adds, the technical challenges of brain magnetic resonance imaging in the presence of deep brain stimulation electrodes should be addressed as well.
One of the study's key findings – that generally-applied electrophysical therapeutic effects show regional significance through interaction with brain pathophysiology – has implications for other electrically-based brain treatments, such as deep brain stimulation and transcranial magnetic stimulation. "We demonstrate that unfocused electrical current changes a highly specific set of brain structures that are well-known to be implicated in mood disorders," Draganski tells Medical Xpress. "The supposition here is that either the applied electrical current, or the resulting epileptic seizure, interact with particular dysfunctional networks, resulting in the specific pattern of structural changes."
Although uni- and bipolar disorders respond differentially to ECT and its associated local brain-volume changes, in the current study both uni- and bipolar disorder patients benefitted equally well from ECT. "Our knowledge about these two nosological," or diagnostically classified, "entities is still limited," Draganski notes. "Departing from the non-biological classification of diseases according to DSM IV or V, we much more see the two disorders as parts of a spectrum. Previous studies have highlighted a differential, but partially overlapping pattern of brain structure changes in uni- and bipolar disorder patients." Nevertheless, Draganski acknowledges that there is no clear answer on the question about "nature and nurture" of these changes – and why changes in different brain areas are associated with clinical outcome prediction in the two remains speculative.
Indeed, more neurobiologically-precise imaging and thereby stimulation might provide seizure-free neurotrophic effects that result in the same benefits as ECT – that is, increased rates of neurogenesis, synaptogenesis, and glial proliferation, particularly in the hippocampus. "Current improvements in magnetic resonance imaging (MRI) technology providing higher image resolution and more insight in brain tissue properties underlying MR signal changes will revolutionize the field," Draganski says. "This will clearly help us reaching our scientific goals of distinguishing between the contribution of cellular and extracellular components to the demonstrated brain volume changes. Extensive clinical research on the behavioral effects of ECT protocol changes will also help differentiating between factors contributing to clinical improvement from nuisance by-effects."
Moving forward, the researchers will focus on developing paradigms for inferring causality – that is, trying to answer the remaining open questions about differential effects in uni- and bipolar disorders, effects of age, ECT application protocols and interaction with specific pharmacological treatment to create reliable biomarkers for prediction of clinical outcome.
"Currently we work on developing new MRI techniques based on well-established biophysical models to go beyond the descriptive nature of our findings on brain anatomy changes," Draganski illustrates. "The aim is to quantify brain tissue properties – myelin, iron, free tissue water – and provide straightforward neurobiological interpretation of our MRI results rather than inferences based on changes in brain volume or cortical thickness."
In general," Draganski concludes, "there are implications of our findings for both basic and clinical neurosciences. Psychiatrists will have stronger arguments to make use of ECT in mood disorder patients refractory," or resistant, "to other forms of treatment, and basic neuroscientists will take on the challenge to investigate the neurobiological mechanisms of ECT at molecular, cellular and systems levels."
More information: Electroconvulsive therapy-induced brain plasticity determines therapeutic outcome in mood disorders, Proceedings of the National Academy of Sciences vol. 111 no. 3, 1156-1161, doi:10.1073/pnas.1321399111
Journal information: Proceedings of the National Academy of Sciences
© 2014 Medical Xpress. All rights reserved.