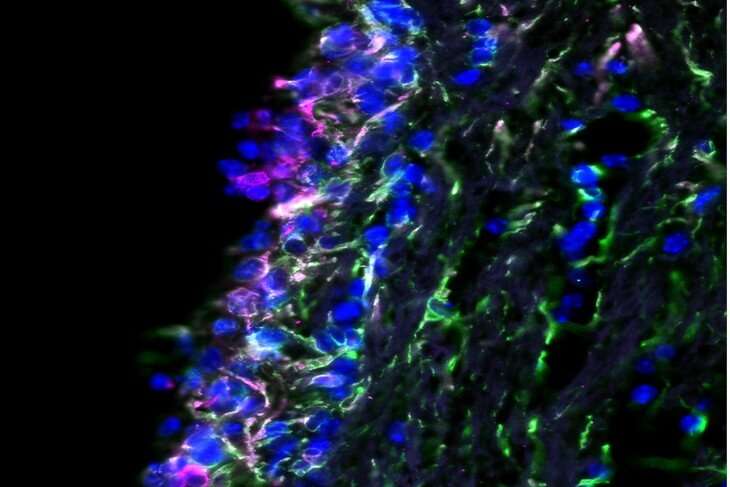
College of Medicine researchers examined the barrier between spinal fluid and brain to look for evidence of infection. Credit: Penn State College of Medicine
A genetic modification in the 'coat' of a brain infection-causing virus may allow it to escape antibodies, according to Penn State College of Medicine researchers. They say testing people for this and other viral mutations may help identify patients at risk for developing a fatal brain disease.
Dr. Aron Lukacher, professor and chair of the Department of Microbiology and Immunology at the College of Medicine, and Susan Hafenstein, professor of medicine and microbiology and immunology at the College of Medicine and professor of biochemistry and molecular biology at Penn State Eberly College of Science, co-led a research team that used high-resolution microscopy to study the capsid, or outer shell of mouse polyomavirus (MuPyV). This virus is a genetic model of JC polyomavirus (JCPyV), which is present and harmless in most people and can cause progressive multifocal leukoencephalopathy (PML), a brain disease, in people taking immunosuppressive therapies.
Genetic mutations in the capsid of JCPyV are common in PML patients and scientists have struggled to understand whether they allow the virus to infect brain cells or whether the resulting changes allow the virus to evade elimination by antiviral antibodies and then cause brain infection. Lukacher and Hafenstein studied the mouse equivalent of a common genetic mutation in JC polyomavirus to try and better understand how it may cause PML.
"Not much is known about how this particular genetic mutation in the JC polyomavirus capsid leads to PML," Lukacher said. "It has been detected in the blood, cerebrospinal fluid and brain tissues of PML patients but not in their urine. This unmutated virus typically sits dormant in the kidneys of healthy people, which got us wondering how this particular mutation contributes to disease progression."
The researchers introduced a genetic mutation in the MuPyV capsid similar to one found in JCPyV and conducted a series of experiments to compare outcomes between MuPyV and the altered virus. The virus mutates by swapping out one amino acid, the chemical ingredients used to build the capsid, for another. They found the virus was still able to cause central nervous system infection and hydrocephalus, or brain swelling.
To study how the mutation allows the virus to evade antibodies, the research team, including doctoral student Matthew Lauver and medical scientist training program student Daniel Goetschius, used cryogenic electron microscopy to determine the 3-D, atomic resolution structure of the virus particles bound to monoclonal antibodies. The results of their analyses were published in the journal eLife.
The team examined the structural features to see how the monoclonal antibodies recognize the virus capsid and neutralize it. They found that the capsid mutation prevents the monoclonal antibody from being able to interact with the virus, increasing the chances that the virus can infect the brain when patients become immune-suppressed.
"We studied how other mutations affected MuPyV and found many of them result in impaired kidney and retained brain viral infection," said Lukacher, a Penn State Cancer Institute researcher. "However, only a few of these result in the ability of the virus to evade the immune response."
According to Lukacher, more research is needed to determine which JCPyV mutations cause the virus to evade antibodies. He said the goal would be to develop screenings for patients with multiple sclerosis receiving immune-modulating therapies, as well as those immune-compromised by cancers and AIDS, to see who might be at increased risk for developing PML.
More information: Matthew D Lauver et al. Antibody escape by polyomavirus capsid mutation facilitates neurovirulence, eLife (2020). DOI: 10.7554/eLife.61056
Journal information: eLife
Provided by Pennsylvania State University