How some prostate tumors resist treatment—and how it might be fixed
Hormonal therapies can help control advanced prostate cancer for a time. However, for most men, at some point their prostate cancer eventually stops responding to further hormonal treatment. This stage of the disease is called androgen-insensitive or castration-resistant prostate cancer. In a study published March 18 in Cancer Cell, a team led by researchers at Sanford-Burnham Medical Research Institute (Sanford-Burnham) found a mechanism at play in androgen-insensitive cells that enables them to survive treatment. They discovered that a protein called Siah2 keeps a portion of androgen receptors constantly active in these prostate cancer cells. Androgen receptors—sensors that receive and respond to the hormone androgen—play a critical role in prostate cancer development and progression.
Based on this new information, Siah2 could make a promising biomarker for tracking a prostate cancer patient's response to therapy. Inhibiting Siah2's interaction with the androgen receptor complex might also provide a new method for re-sensitizing castration-resistant prostate tumors to hormone therapy.
Siah2 removes the brake on androgen receptors
"Prostate tumors become castration-resistant by using diverse ways to modify androgen receptor to become constantly active. In this study, we demonstrate how this happens through a previously unknown mechanism orchestrated by Siah2. Surprisingly, it turns out that only a fraction of all androgen receptors are altered in castration-resistant tumors," said Ze'ev Ronai, Ph.D., associate director of Sanford-Burnham's National Cancer Institute-designated Cancer Center, scientific director of the Institute's La Jolla campus, and senior author of the study.
Normally, androgen receptors are kept in check by an inhibitor called NCOR1. This study revealed that, in castration-resistant prostate tumors, Siah2 tags the NCRO1-androgen receptor complex for degradation. That removes the brake, allowing the recycling of inactive androgen receptor to active status. As a result, prostate cancer cells produce more active androgen receptors, which render them resistant to hormone therapy.
Clinical relevance
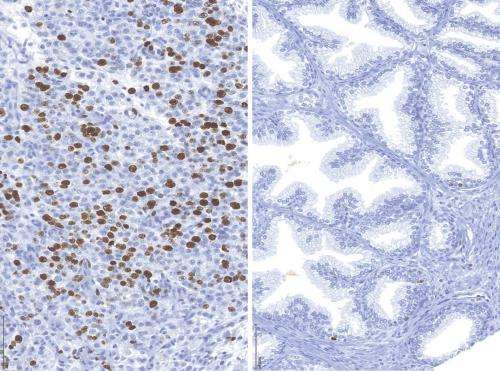
Ronai and colleagues wondered if Siah2 plays the same role in real-life castration-resistant prostate cancer as they had observed in the lab. Using samples provided by collaborators at the Vancouver Prostate Centre at the University of British Columbia, the team determined that human castration-resistant prostate tumors have abnormally high levels of Siah2 and select androgen receptor targets. This finding underscores the clinical significance of the castration-resistance mechanism they uncovered.
Ronai and his team also looked at what happens when they inhibit Siah2. To do this, they used three different animal models. In each case, inhibiting Siah2 restored prostate tumors' sensitivity to hormone therapy. With Siah2 out of the picture, prostate tumors regressed during hormone therapy.
"We see Siah2 not only as a biomarker—a way to track the development and progression of castration-resistance—but also as a potential therapeutic target for prostate cancer," explained Jianfei Qi, Ph.D., staff scientist in Ronai's lab and first author of the paper.











