Unraveling the largest outbreak of fungal infections associated with contaminated steroid injections
Investigators from the Centers for Disease Control and Prevention (CDC) describe pathologic findings from 40 case reports of fungal infection in patients who had been given contaminated epidural, paraspinal, or intra-articular (into joints) steroid injections and correlate these findings with clinical and laboratory data. The report, published in the September issue of The American Journal of Pathology, alerts clinicians and the general public to the catastrophic dangers of contaminated epidural injections.
In September 2012, CDC began hearing multiple reports of fungal meningitis in patients following epidural steroid injections. By June 2013, 745 people had confirmed infections and 58 had died, making this the largest reported outbreak of infections associated with epidural and intra-articular injections.
After intensive investigation, the contamination was traced to more than 17,000 vials from three contaminated lots of preservative-free methylprednisolone acetate (MPA) originating from a single compounding pharmacy. More than 13,000 people were injected with the potentially contaminated drug. Most cases were attributable to Exserohilum rostratum, a dark-colored environmental mold that rarely infects humans.
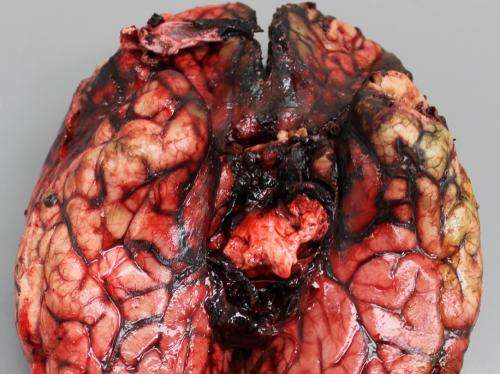
Researchers, including the CDC's Exserohilum Infections Working Group, report that of 40 cases reviewed, 16 were fatal, and all except two fatal cases had a clinical diagnosis of meningitis. Autopsy examination showed extensive hemorrhage and necrosis (tissue decay) around the base of the brain and thrombi (clots) involving the basilar arterial circulation.
Tissue specimens from infected individuals showed inflammation of the leptomeninges (thin membranes lining the brain) and blood vessel walls within the brain. Distinctive abnormalities were observed around blood vessels, and fungus was found around and within arterial walls. Interestingly, fungus deep within the brain tissue itself was found in only one case.
Similar pathologic findings were seen at the epidural injection site. Fungus was not found in tissue samples taken from the heart, lung, liver, or kidney.
Investigators wondered why fungus injected in the spinal region should target the base of the brain. "The observation of abundant fungi in the perivascular tissues, but relatively low numbers of fungi inside blood vessels, suggests migration of fungus into, rather than out of, vessels at this location. This supports the hypothesis that Exserohilum migrates from the lumbar spine to the brain through the cerebrospinal fluid with subsequent vascular invasion, rather than migration through the vasculature," suggests Jana M. Ritter, DVM, a veterinary pathologist at the CDC's Infectious Diseases Pathology Branch.
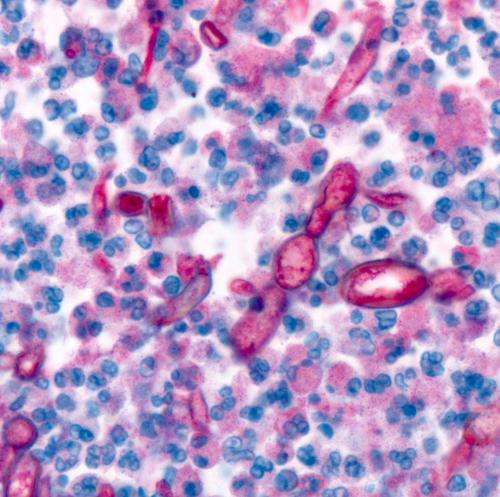
In addition to characterizing the histopathology seen in this outbreak, the authors also provide practical information for pathologists, including an evaluation of various diagnostic methods to detect the fungal infection in tissues. Polyfungal immunohistochemistry (IHC) in formalin-fixed paraffin-embedded tissues (FFPE) was found to be the most sensitive method. IHC identified fungus in 100% of cases, compared with 43% by standard hematoxylin-eosin (H&E) and 95% with Grocott's methenamine silver (GMS) stains. Factors that may affect cellular inflammatory patterns and fungal concentration are discussed, and the authors note that their findings may reflect the simultaneous introduction of the fungus along with the steroid.
More information: "Exserohilum infections associated with contaminated steroid injections: A clinicopathologic review of 40 cases," by Jana M. Ritter, Atis Muehlenbachs, Dianna M. Blau, Christopher D. Paddock, Wun-Ju Shieh, Clifton P. Drew, Brigid C. Batten, Jeanine H. Bartlett, Maureen G. Metcalfe, Cau D. Pham, Shawn R. Lockhart, Mitesh Patel, Lindy Liu, Tara L. Jones, Patricia W. Greer, Jeltley L. Montague, Elizabeth White, Dominique C. Rollin, Cynthia Seales, Donna Stewart, Mark V. Deming, Mary E. Brandt, Sherif R. Zaki, and the Exserohilum Infections Working Group (DOI: 10.1016/j.ajpath.2013.05.007). It appears in The American Journal of Pathology, Volume 183, Issue 3 (September 2013)
















