How to turn the bad guys good in hardened arteries
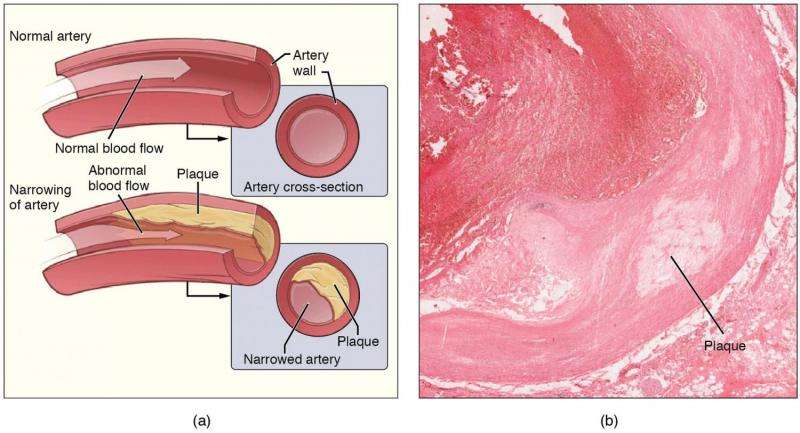
Hardening of the arteries, or atherosclerosis, is one of the most common cardiovascular diseases and is a common feature of ageing but it is not good news. When complex, calcified fatty plaques accumulate and develop up on the inner surface of major arteries, it pushes up the risk of heart attack and stroke.
That's why Conway Fellow, Dr Orina Belton is figuring out how targeting a key cell of the immune system could change the nature of plaques, and possibly even reduce the damage. "Hardening of carotid arteries is a progressive inflammatory disease and is a major risk factor for clinical events such as a heart attack and stroke. Ageing, lifestyle, high blood pressure, high cholesterol and diabetes are major drivers of this disease," explains Dr Belton, who is a senior lecturer in Pharmacology and Head of Research & Innovation at the UCD School of Biomolecular and Biomedical Science.
"But by the time a person is diagnosed with atherosclerosis, the plaques are often well established and there are currently no therapies that can regress the established plaques."
Dr Belton has been looking at how a type of immune cell called a macrophage is involved in plaque building, and how those cells could be 'programmed' to help plaques regress instead. Macrophages come in initially as 'good Samaritans' and soak up excess cholesterol in plaques, but in an atherosclerotic environment the cells dump the fat into the artery, sustaining the disease and contributing further to hardening, she explains.
Her work has been finding that administering a precise ratio of conjugated linoleic acids (CLAs) seems to alter how the macrophages behave. "The macrophages change function and they move away from the plaque," says Dr Belton.
Pre-clinical work suggests that 'reprogramming' the macrophages with this blend of lipids reduces the size of plaques, but the lipids themselves would not form the basis of a therapy, so a major aim of Dr Belton's research is to identify how the macrophages get reprogrammed. "We have been uncovering some novel biochemical pathways that get turned on to make this happen," she says. "And when you fundamentally alter the macrophage you change the microenvironment of the plaque, and this is what we believe can cause the plaque to shrink or regress."
Dr Belton is also looking at genes expressed in blood samples and plaques that have been surgically removed from consenting patients at the St. Vincent's University Hospital to compare patients who have had a cardiac event or stroke and patients who have hardened arteries but no 'events'.
"The ultimate goal is if to find a way to specifically target that macrophage response in atherosclerosis so that when you see people with risk factors at the start of the disease you could intervene earlier and stop the progression of the disease, that would be really significant," she says. "And if this macrophage switch happens in other inflammatory diseases too, like chronic kidney disease or diabetes, then understanding the trigger for that switch would have a huge impact."


















