Q&A on hepatitis C epidemic in Appalachian states
A recent study released by the Centers for Disease Control and Prevention (CDC) found that hepatitis C cases across four Appalachian states—Kentucky, Tennessee, West Virginia, and Virginia—more than tripled between 2006 and 2012. The study is the first from the CDC to link the rise in hepatitis C to an increase in injection drug use and raises concern that a single person could become the "Typhoid Mary of HIV."
UMass Law Associate Professor Margaret Drew, Director of Clinics and Experiential Learning at the Law School, has been named a Bellow Scholar by the Association of American Law Schools (AALS) and received a research award to support a cross-college project that will assess the unmet legal, medical and other needs of HIV-positive individuals living in the SouthCoast region in Massachusetts.
"Building Community Capacity for HIV-Positive Individuals in SouthCoast, Massachusetts" is the project for which Margaret received the fellowship. The research also received $32,000 through the University of Massachusetts President's Creative Economy Initiatives Fund to establish multi-disciplined community partnerships to reduce physical, social, healthcare, and legal barriers for HIV-positive individuals living in New Bedford and Fall River; and to contribute to the workforce development of community health workers in the SouthCoast region. The project is a partnership between Dr. Caitlin Stover of UMass Dartmouth's College of Nursing and UMass Law Lecturer Jason Potter Burda.
Professors Drew, Burda, and Stover discuss the CDC report and spillover issues (legal, medical, etc.) that these states and the communities within them are experiencing.
According to a new report issued by the U.S. Centers for Disease Control and Prevention Hepititis C infections rose 364 percent from 2006 to 2012 in Kentucky, Tennessee, Virginia and West Virginia. How surprising should we be by this substantial increase?
MD: We should not be surprised by these findings. Those living in rural areas and in poverty would have the most difficulty in obtaining adequate assistance with the resulting mental and physical health needs that addiction brings. The southern states have had higher rates of infection of both Hep-C and HIV than other regions. But Hep-C and HIV infections are increasing all over the country, primarily due the increase in intravenous drug use. The SouthCoast is experiencing significant increases in infections of Hep-C and HIV (frequently these are concurrent diagnoses) which is why our team decided to focus our research in this area. We will be assessing the unmet legal, health and other needs of those living with HIV. We expect that many of the HIV+ individuals we interview will also be living with Hep C.
How significant is it that this report is the first CDC study to link the rise in hepatitis C to an increase in injection drug use?
CS: I think that this is notable because the CDC is starting to recognize that injection drug use is not responding to public health education efforts as it continues to be on the rise, especially in urbanized cities. Instead of turning away from it, the CDC it is acknowledging the problem both in rural and urban areas. This will ultimately help in reducing the stigma faced by the intravenous drug use (IDU) population. Once society can reduce the stigma (both actual and perceived), the real work of reducing Hepatitis C and other diseases transmitted via IDU can begin.
What are the spillover issues (legal, medical, etc.) that these states and the communities within them are experiencing?
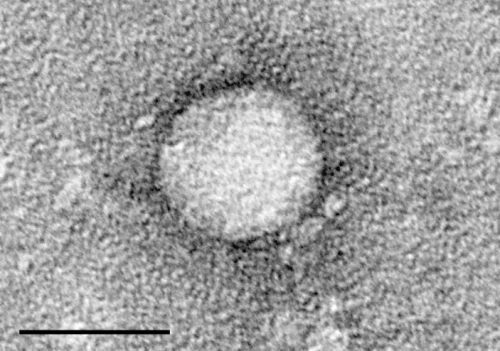
JPB: One of the medical and attendant policy-related issues is that the Hepatitis C virus (HCV) itself, unlike HIV, sustains its viability long after it is exposed to air. For example, HCV can survive on a used syringe for months after injection depending on the conditions. This puts into perspective the necessity of safe syringe disposal and clean syringe access. Nonetheless, successful harm reduction programs, such as syringe exchanges staffed by community health workers trained to link addicts to additional treatment, are unable to seek federal funding due to the federal ban on funding for needle exchange programs. So, states wishing to operate these services must fund the programs themselves or seek the help of private organizations. Access to successful treatment of Hep-C is a barrier to those who are uninsured or inadequately insured. Because of the connection between poverty and Hep-C and HIV, our research may uncover links between the infectious diseases and inadequate housing conditions, difficulties in accessing benefits, as well as discrimination due to stigma.















