New research raises questions about using certain antibiotics to treat 'superbug' MRSA
A new study sheds light on how treatment of the "superbug" known as MRSA with certain antibiotics can potentially make patients sicker. The findings by Cedars-Sinai scientists, published today in the journal Cell Host & Microbe, could have implications for managing the bug, a virulent form of the common staph infection that can be difficult to control.
MRSA, or methicillin-resistant Staphylococcus aureus, recently made the news when New York Giants tight end Daniel Fells received treatment for it. MRSA has long caused problems in the sports world, especially in football and wrestling, in which athletes have close body contact. But anyone can contract the infection when the bacteria enter the body through a cut, sore, catheter or other means.
MRSA causes more than 80,000 invasive infections and 11,000 related deaths per year, according to 2011 figures from the federal Centers for Disease Control and Prevention. Fatalities are more likely when the bacteria enter the bloodstream or lungs, according to George Liu, MD, PhD, co-senior author of the Cell Host & Microbe article. "It is one of the biggest antibiotic-resistant pathogens in the US," said Liu, a pediatric infectious diseases physician at Cedars-Sinai's Maxine Dunitz Children's Health Center and the F. Widjaja Inflammatory Bowel and Immunobiology Research Institute.
The research team cautioned that their findings were based on laboratory studies of mice and that the results need to be carefully evaluated in human subjects for validation.
"Based on this research, clinical studies are warranted," said study author Sabrina Mueller, PhD. "However, pending the outcome of those studies, physicians should follow current national guidelines set by the Infectious Diseases Society of America for antimicrobial treatment of staph infections."
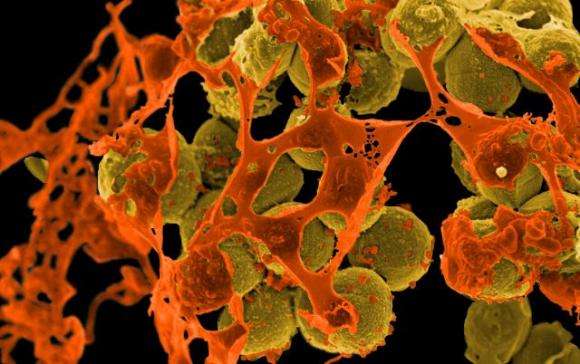
Although many studies have established that MRSA infections cause more severe diseases compared with normal staph infections, what makes MRSA so pathogenic is not entirely clear. The Cedars-Sinai scientists found one answer in the name of the superbug—methicillin-resistant. In laboratory mice, treatment with antibiotics similar to methicillin, called beta lactams, caused the MRSA bacteria to build cell walls that are highly inflammatory and damaging to tissues.
The scientists explained that beta-lactam antibiotics kill normal staph bacteria by inactivating their cell-wall-making enzymes. But one of these enzymes, PBP2A, which is induced when MRSA is exposed to beta-lactam antibiotics, is not rendered inactive by the antibiotics. In fact, PBP2A allows the superbug to continue making its cell wall. Further, the cell wall's structure differs from that of normal staph, and not in a good way. "This altered cell wall induces a powerful inflammatory response," said the study's co-senior author, David Underhill, PhD, associate director of the Division of Immunology Research in the Cedars-Sinai Department of Biomedical Sciences and the Janet and William Wetsman Family Chair in Inflammatory Bowel Disease. "In mice infected with MRSA, induction of PBP2A with methicillin led to more inflammation and pathology."
In other words, the mice became sicker.
The authors said their study findings in mice raised the possibility that prescribing beta-lactam antibiotics to treat infections in humans may worsen the infection, should the source prove to be MRSA. The potential dilemma for physicians is that beta-lactam antibiotics' overall effectiveness often makes them the first line of defense when the origin of a severe infection is unknown. And it can take a day or two to culture MRSA, making early diagnosis difficult, Liu said.
"There is much work ahead of us before we can make a firm recommendation about the advantages or disadvantages of treatment with beta-lactam antibiotics," Liu said.
More information: Cell Host & Microbe, Müller et al.: "Poorly Cross-Linked Peptidoglycan in MRSA Due to mecA Induction Activates the Inflammasome and Exacerbates Immunopathology" dx.doi.org/10.1016/j.chom.2015.10.011


















