An unprecedented TB outbreak in Papua New Guinea
An outbreak of multidrug resistant tuberculosis (MDR-TB) in Papua New Guinea may well become a replay of the disastrously delayed response to the West African Ebola pandemic, says Jennifer Furin, Harvard Medical School lecturer on global health and social medicine, in a commentary she co-authored with Helen Cox, senior lecturer in the Division of Medical Microbiology at the University of Cape Town, South Africa. The commentary was published in Lancet Respiratory Medicine on March 23 to coincide with World TB Day, which is today, March 24.
Harvard Medicine News spoke to Furin to learn more about the situation in the island province of Daru, just north of Australia in the southwestern Pacific.
HMN: What's happening on Daru?
JF: Currently, on Daru Island in Papua New Guinea, there is a significant and ongoing outbreak of MDR-TB. It is spreading throughout the country and could possibly move to Australia.
HMN: How does it compare to other outbreaks globally?
JF: Conservative estimates show that 1 percent of the population of Daru is sick with MDR-TB. This translates to about 150 cases per year in a population of 15,000. As a point of comparison, an outbreak on nearby Chuuk Island, one that the CDC was able to get under control, had 26 cases in a population of 108,000.
In one community in South Africa, Khayelitsha, there are about 200 MDR-TB cases a year, with a population of about 400,000 and an HIV prevalence above 20 percent.
Since Daru has almost no HIV—which greatly increases the risk of contracting MDR-TB—the number of cases there is even more staggering.
HMN: How did things get so bad?
JF: A number of factors. For example, some MDR-TB patients from Papua New Guinea who had been getting treatment in Australia were sent back home—many of them to Daru—in order to give them care closer to their families.
This was well-intended, but available care was limited on Daru. Once the infection started spreading on the island, it became difficult to stop.
Because the islanders are poor, people share accommodations—often crowding 20 people into a single room. In addition, there were few diagnostic and treatment services available on the island.
Although services have improved over the years, they have not improved fast enough to keep up with the current outbreak of the disease.
Finally, international health and policy advisors to Papua New Guinea have not given the health program leaders advice that will help them to stop this outbreak.
HMN: You've called the outbreak a "time bomb." Why do you use that term?
JF: Because one does not notice the full devastation of the event right away.
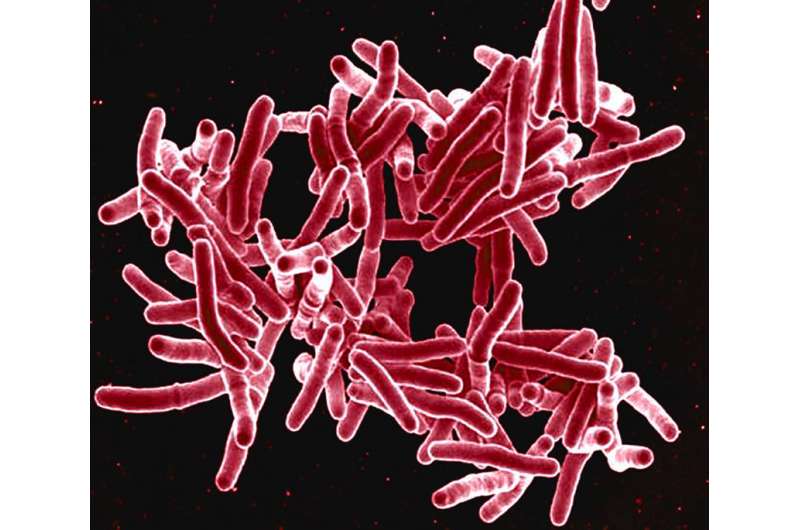
With TB, people can become infected with the bacterium and not become sick until months or years later.
Someone with TB can cough in a room and expel the bacterium, where it will remain infectious for hours. Hundreds of people could breathe in those infectious organisms and not know for some time that they have been infected.
Because infection is not readily apparent, TB is much more frightening than diseases we tend to hear a lot about, such as Ebola, where infection tends to lead rapidly to disease development.
But when I describe the situation as being like a time bomb, I also mean that if we act to do something now, we might be able to defuse the situation.
HMN: What would it take to stem this disease in Papua New Guinea?
JF: There needs to be a massive influx of resources—human and financial—into the country. Although the government has put together an excellent plan to stop the outbreak, it does not have the funding or the staff to put the plan into action. And it is likely that the situation on Daru Island is also happening elsewhere in the country.
Urgent action on a large scale is needed now to support the planning done by the government. These plans include active case finding, rapid diagnosis and treatment with optimal therapy and preventive measures for those who have been exposed to pathogens.
HMN: TB is a treatable disease, but it still kills more than a million people every year. What does the reaction to this outbreak say about efforts to get to zero deaths?
JF: According to the new WHO "End TB Strategy," we are supposed to eliminate TB by 2030, which is only 14 years away. But we don't know how to actually eliminate TB; we have tried to control only the impact the disease has on the world's populations.
This control strategy has been highly ineffective: TB is once again the infectious disease that causes the highest mortality among adults around the world, even though it is curable.
But if we are serious about ending TB in just a decade and a half, we have to start actually eliminating it. Daru would be the ideal place to make this happen, since the number of cases is manageable and the geographic location where the cases are occurring is small.
However, so far there has been no real attempt to try to eliminate the disease on Daru. Since the global health organizations cannot even commit to eliminating MDR-TB on Daru, it is hard to believe that we will be successful in getting to zero anytime soon.
More information: Jennifer Furin et al. Outbreak of multidrug-resistant tuberculosis on Daru Island, The Lancet Respiratory Medicine (2016). DOI: 10.1016/S2213-2600(16)00101-6















