Engineering electrically conducting tissue for the heart
Patients with complete heart block, or disrupted electrical conduction in their hearts, are at risk for life-threatening rhythm disturbances and heart failure. The condition is currently treated by implanting a pacemaker in the patient's chest or abdomen, but these devices often fail over time, particularly in infants and small children who must undergo many re-operations. Researchers at Children's Hospital Boston have now taken preliminary steps toward using a patient's own cells instead of a pacemaker, marking the first time tissue-engineering methods have been used to create electrically conductive tissue for the heart.
Results appear in the July issue of the American Journal of Pathology (published online on June 19).
In complete heart block, electrical signals cannot pass from the heart's upper chambers (atria) to the lower chambers (ventricles), leading to heart failure. In normal hearts, electrical impulses move first through the atria, then pause at the atrioventricular (AV) node. Then, after a short delay that allows the ventricles to fill with blood, the AV node releases the impulses, which move through the ventricles causing them to contract. In this way, the beats of the atria and ventricles are synchronized.
Investigators led by Douglas Cowan, PhD, a cell biologist in Children's Department of Anesthesiology, Perioperative and Pain Medicine, wanted to create a biological substitute for the AV node that would work in patients who have defective atrioventricular conduction. "The idea was that rather than using a pacemaker, we could create an electrical conduit to connect the atria and ventricles," Cowan says.
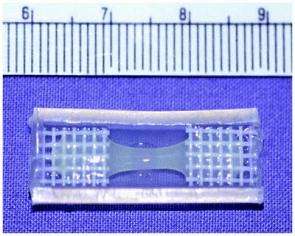
Cowan's team, including first author Yeong-Hoon Choi in Children's Department of Cardiac Surgery, obtained skeletal muscle from rats and isolated muscle precursor cells called myoblasts. They "seeded" the myoblasts onto a flexible scaffolding material made of collagen, creating a 3-dimensional bit of living tissue that could be surgically implanted in the heart.
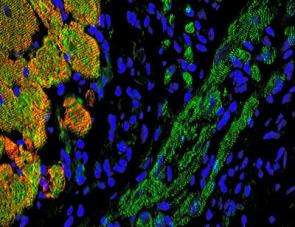
The cells distributed themselves evenly in the tissue and oriented themselves in the same direction. Tested in the laboratory, the engineered tissue started beating when stimulated electrically, and its muscle cells produced proteins called connexins that channel ions from cell to cell, connecting the cells electrically.
When the engineered tissue was implanted into rats, between the right atrium and right ventricle, the implanted cells integrated with the surrounding heart tissue and electrically coupled to neighboring heart cells. Optical mapping of the heart showed that in nearly a third of the hearts, the engineered tissue had established an electrical conduction pathway, which disappeared when the implants were destroyed. The implants remained functional through the animals' lifespan (about 3 years).
"The advantage of using myoblasts is that they can be taken from skeletal muscle rather than the heart itself--which will be important for newborns whose hearts are so tiny they cannot spare any tissue for the biopsy--and that they're resistant to ischemia, meaning they can go without a good blood supply for a relatively long period of time," Cowan says.
Cowan and his team are now working with a large-animal model that more closely simulates pediatric heart block. Further studies will seek to create tissue-engineered grafts that behave more like a natural AV node, for example by providing a built-in delay before sending electrical signals to the ventricles. The team is investigating whether other cell types, such as stem cells derived from muscle or bone marrow, might be made to behave more like AV node cells.
Complete heart block is present in about 1 in 22,000 births. It can also result from congenital heart disease, through an injury or scar tissue from heart surgery, or as a side effect of medications. In adults, pacemakers are a good solution, but in children, they carry a greater risk of heart perforation and clot formation. In addition, pacemakers only last 3 to 5 years in children, and the leads must be replaced frequently, requiring many repeat operations. In very small babies, the pacemaker leads must be positioned on the heart surface, resulting in even greater failure rates.
Cowan envisions a future in which a child with heart block would receive a conventional pacemaker, but also receive an implant of engineered, electrically conducting tissue that would grow along with the child. The pacemaker, acting as a backup, would start functioning only if the biological implant failed, prolonging its useful life.
Source: Children's Hospital Boston















