NSAID increases liver damage in mice carrying mutant human gene
Alpha-1-antitrypsin deficiency isn't a term that rolls right off the tongue. But people diagnosed with this genetic disorder learn its potential effects well. They know they shouldn't smoke or be around smokers because they are at increased risk for developing emphysema at a young age. In addition, some patients with alpha-1-antitrypsin (AT) deficiency can develop serious liver disease. But predicting which of them are at risk for liver disease is not yet possible.
Now research performed at Washington University School of Medicine in St. Louis sheds light on the mechanisms that contribute to liver disease in alpha-1-AT deficiency patients. Using an experimental mouse model of the disorder, the researchers investigated the effects of a non-steroidal anti-inflammatory drug (NSAID) on liver injury. An estimated 15 to 20 million people in the United States take NSAIDs like ibuprofen and naproxen on a long-term basis.
The findings, published in the October issue of the journal Hepatology, show that the NSAID indomethacin (Indocin), administered at doses typically nontoxic to mice, significantly increased liver damage in the experimental mice.
The mice carried a mutated form of the human alpha-1-AT gene (called the alpha-1-ATZ gene), the most common form of the gene associated with the development of liver disease in people with alpha-1-AT deficiency. Greater expression of the mutant alpha-1-ATZ gene and increased amounts of alpha-1-ATZ protein in the liver accompanied the increase in liver injury in the experimental mice given the NSAID.
"These data demonstrate that environmental factors such as drug administration can affect the development of liver injury in this animal model," says lead author David Rudnick, M.D., Ph.D., assistant professor of pediatrics and of molecular biology and pharmacology. "And they raise the possibility that NSAIDs could have similar effects on gene and protein expression and perhaps on liver injury in people with alpha-1-AT deficiency."
Approximately 1 in 2,000 individuals has alpha-1-AT deficiency. Rudnick points out that even though alpha-1-AT deficiency is the most common genetic indication for pediatric liver disease and liver transplantation, a study to investigate whether NSAIDs affect human alpha-1-AT patients may not be feasible because of the disorder's relative rarity.
"But I tell my patients with any form of chronic liver injury they should avoid NSAIDs," says Rudnick, a pediatric gastroenterologist at St. Louis Children's Hospital. "The drugs have an established potential hepatotoxicity. I would say alpha-1-AT deficiency liver disease is another example where these drugs should be avoided."
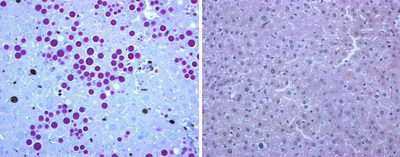
Normally, the liver secretes alpha-1-AT protein into the bloodstream, but the abnormal protein, alpha-1-ATZ, can get "stuck" in liver cells. Liver biopsies of alpha-1-AT deficiency patients reveal that their liver cells have numerous globules containing alpha-1-ATZ protein.
The defective alpha-1-ATZ doesn't reach the lungs, where alpha-1-AT normally regulates enzymes that digest protein. Loss of alpha-1-AT's regulation of protein-digesting enzymes in the lungs can result in tissue damage and emphysema.
In ways not yet entirely understood, accumulation of alpha-1-ATZ in the liver can lead to both liver damage and liver cancer. In the mice carrying the human alpha-1-ATZ gene, the NSAID indomethacin not only caused liver cells to accumulate even more of the abnormal alpha-1-ATZ protein but also to proliferate or multiply faster than usual — a hallmark of liver response to injury.
People who have alpha-1-AT deficiency vary widely in the severity of liver injury: some patients never have liver problems while others will require a liver transplant before they are two years old. Only 10 to 20 percent of infants with alpha-1-ATZ genes will develop clinically overt liver damage.
"We don't yet know the mechanism accounting for such wide variability in this disorder, but other genetic and environmental factors must contribute," Rudnick says. "The effect of indomethacin on these transgenic mice suggests that NSAIDs may be an example of such an environmental influence."
Source: Washington University School of Medicine in St. Louis





















