Brain cells need microRNA to survive
There are lots of things that brain cells need to survive. Add to that list microRNAs. New research from Rockefeller University shows that neurons that cannot produce microRNAs, tiny single strands of RNA that regulate the expression of genes, slowly die in a manner similar to what is seen in such human neurodegenerative disorders as Alzheimer’s and Parkinson’s diseases.
In the July issue of the Journal of Experimental Medicine, the researchers say that although no one has yet found microRNAs to be involved in any disease, their study in mice shows that these tiny snippets of RNA are essential for survival of mature neurons.
“This research tells us that microRNAs are needed if certain neurons are to function and survive, and that means they are likely involved in survival of other neurons as well,” says the study’s senior investigator, Paul Greengard, head of the Laboratory of Molecular and Cellular Neuroscience. “That leads us to hypothesize that abnormalities in microRNA expression might be causing or modifying disease progression.”
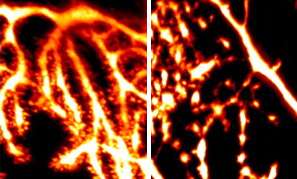
The researchers specifically found that mice engineered to stop expression of microRNAs in cerebellar cortex neurons after birth experienced a slow decline in function, resulting in death of the neurons, known as Purkinje cells. Because this brain area helps control motor function, mice without functioning Purkinje neurons could no longer walk correctly.
Since the use of these particular cells was a model system testing deletion of microRNAs, the results can likely be extended to other types of neurons, such as those involved in memory and higher thinking, says the study’s lead author, Anne Schaefer, a postdoctoral fellow in Greengard’s lab. These findings are “very exciting,” she says. “There was no evidence that mature neurons, which are differentiated and don’t divide any more, would require microRNAs for their function or survival.”
Since their discovery in 1993, microRNAs have been found to be powerful regulators of gene expression, but mainly in cells that are developing. Differentiating neurons expressed a large variety of microRNAs, Schaefer says, and development stops if microRNAs cannot function. While these bits of RNA were also known to exist in mature neurons, no one knew if they play any role in the life of adult neuronal cells, she says.
To find out what role they do play, the research team cross-bred three different kinds of mice. One, created by co-author Dónal O’Carroll, in the Rockefeller Laboratory of Lymphocyte Signaling, is known as a “Dicer conditional” mouse. It gives researchers the ability to delete a gene known as Dicer, whose protein is required to produce microRNAs. They cross-bred these mice with another line, produced by researchers at the University of Hong Kong, that expresses a protein, Cre-recombinase, that inactivates Dicer in postnatal Purkinje cells. The offspring of these mice were then bred with a mouse engineered to express green fluorescent proteins when Dicer is deleted. In this way, the researchers were able to follow Dicer deletion and could then test for the presence of different microRNAs known to be expressed in the adult brain.
They found that some microRNAs were deleted right away but that others took longer, and during this time, the cells were basically stable although slowly degenerating. Eventually the “mice showed symptoms reminiscent of those seen in humans with neurodegenerative disorders, and by 18 weeks almost all of the Purkinje cells had died,” Schaefer says.
Whether changes in specific microRNAs contribute to human disorders remains to be seen, she says, but now researchers have ways to test that. They can compare microRNA expression between normal and diseased human brains and they can knock out specific microRNAs in their mouse model to determine which may be playing the more critical roles. “Now we have a roadmap for identification of genes which might be involved in neurodegeneration and that is very exciting,” Greengard says.
Citation: Journal of Experimental Medicine Online: July 2, 2007
Source: Rockefeller University



















