Scientists grow blood vessels for human surgery

Scientists can grow blood vessels in a lab for use in coronary bypass or dialysis, a promising alternative to harvesting from the patient, said a study published on Wednesday.
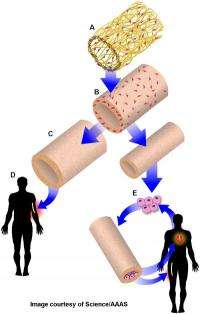
The process involves taking smooth muscle cells from a human cadaver and grafting them onto tubes made of the material used in making dissolvable stitches, called polyglycolic acid.
Within eight to 10 weeks, the tubes degrade and a "fully formed vascular graft" remains, said the research by scientists from Duke University, East Carolina University and Yale University.
The veins have been tested in baboons and dogs. They were not rejected by the animals' bodies and functioned well for six months, said the study, published in the journal Science Translational Medicine.
The bio-engineered vessels could also be stored in saline solution for up to a year, suggesting that one day surgeons could pluck a vein "off the shelf" for use in a sick patient, the study said.
"These can be made ahead of time and then are ready to go whenever they are needed," the paper said.
Clinical trials in humans are expected to begin soon, according to a spokeswoman from Humacyte, a regenerative medicine company based in North Carolina that also contributed to the study and funded the research.
"Currently, grafting using the patient's own veins remains the gold standard," said co-author Alan Kypson of the Brody School of Medicine at East Carolina University.
"But, harvesting a vein from the patient's leg can lead to complications, and for patients who don't have suitable veins, the bio-engineered veins could serve as an important new way to provide a coronary bypass."
The engineered vessels also have "decreased potential for infection, obstruction or clotting," the study noted.
Shannon Dahl, senior director of Scientific Operations at Humacyte, said veins can be made in a variety of sizes for use in different operations.
"We can make the bio-engineered veins in large and small diameter which means they can be used for procedures ranging from hemodialysis for patients with kidney failure and for coronary by-pass," she said.
The National Kidney Foundation says that 320,000 patients require dialysis, and "more than half of dialysis patients lack the healthy veins necessary and must undergo an arteriovenous graft (AV graft) placement" for the procedure.
Around 400,000 coronary bypass procedures are performed annually in the United States, according to the American Heart Association.
(c) 2011 AFP
















