Advice urges wider sharing of heart care decisions
(AP) -- A heart device might save your life but leave you miserable. That awful possibility is the reason for new advice urging doctors to talk more honestly with people who have very weak hearts and are considering pumps, pacemakers, new valves or procedures to open clogged arteries.
Too often, patients with advanced heart failure don't realize what they are getting into when they agree to a treatment, and doctors assume they want everything possible done to keep them alive, says the new advice, published Monday by the American Heart Association and endorsed by other medical groups.
It calls for shared decision making when patients face a chronic condition that often proves fatal and they need to figure out what they really want for their remaining days. If they also have dementia or failing kidneys, the answer may not be a heart device to prolong their lives.
"Patients may feel that the treatment was worse than the disease," said Dr. Larry Allen of the University of Colorado Anschutz Medical Center, who helped draft the new advice.
One of his former patients is an example: a 74-year-old man too weak to go shopping or walk around his neighborhood. He was so miserable that doctors thought he would feel better with a "mini artificial heart" - a $100,000 left ventricular assist device to make his heart pump better.
"Even if it goes well, people are left with an electrical cord coming out of their belly" and a higher risk of stroke and bleeding from the nose or throat, Allen said.
The man suffered bleeding problems, needed a breathing machine and spent 10 weeks in the hospital. He and his wife hated that his device kept him tethered to a power supply or gave him only a few hours of freedom on battery power. Some models last longer.
"They came to us a couple months after he went home and said his quality of life was not what he wished" and asked to have the pump turned off, Allen said. The man died about a year ago.
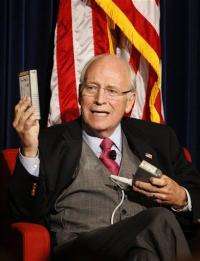
By contrast, former Vice President Dick Cheney, 71, has been living with a heart assist device since the summer of 2010 and reports "doing well for now" in his recent memoir. Cheney, who had the first of five heart attacks at age 37, proudly shows off the long-life batteries he wears in a vest.
"I've gotten used to the various contraptions that are always with me, and I'm working and traveling, I've hunted a time or two, and I have some fishing planned," he wrote in his memoir released last year.
More than 5 million Americans have heart failure, and the number is growing as the population ages. It occurs when a heart becomes too weak - because of a heart attack, high blood pressure or other condition - to pump enough blood. Fluid can back up into the lungs, causing shortness of breath, weight gain, fatigue and swollen ankles.
Many high-tech treatments are available to treat advanced disease. But they usually don't slow its progression, they just keep people from dying. And that means living longer with steadily worsening symptoms. Patients don't often understand that when they agree to gadgets like a $30,000 to $50,000 implanted defibrillator, which shocks a quivering heart back into normal rhythm.
"Defibrillators don't actually make people feel better - it doesn't treat the underlying heart failure. All it does is abort sudden death," Allen said.
More than 100,000 defibrillators are implanted each year in the United States, and one quarter of them are replacement operations because a battery has worn out (they last three to five years). That often is done without reconsidering whether a patient's health has deteriorated so much that the device isn't a good idea, three Harvard Medical School doctors wrote recently in the New England Journal of Medicine.
The new heart association advice takes aim at this problem. It urges:
-An annual talk between heart failure patients and doctors to set treatment goals for the present and for possible emergencies such as cardiac arrest.
-"Milestone" reviews after any big change such as hospitalization, a defibrillator shock, worsening kidney problems or dementia.
-Discussing not just survival gains but also potential problems from devices or treatments, such as side effects, loss of independence, quality of life and obligations on families and caregivers.
-Considering palliative care, which does not mean stopping treatment.
The goal is "not only living long, it's living well. People often make decisions about the `long' without even considering the `well,'" said Jessie Gruman, president of the Center for Advancing Health, a patient advocacy group. The heart association asked Gruman, who has had several cancers and a heart problem, to review the advice from a patient's perspective.
The worst thing is to have no plan or clear goals when an emergency occurs, she said.
"The person who's ill may not have particular cognitive clarity and the caregivers may be upset and exhausted. They just haven't thought it through - they haven't had a chance to think it through. They've never done this before," Gruman said.
Mary Jane Eaton has thought it through. She's 80 and lives in Aurora, Colo., just east of Denver. Twenty years ago, she had a new heart valve put in that is leaking now. She has heart failure and chest pains, probably from clogged arteries. After talks with her cardiologist, Dr. Jennifer Dorosz, she has decided to treat her fluid buildup with higher doses of water pills and not have any more tests or surgery.
"I can't see that I could go through that," she said. "At my age, I just figure you know what, when the Lord's ready for me, he's going to take me. And I don't want to be taken on the operating table."
More information:
Heart Association: www.americanheart.org
Heart failure info: www.nhlbi.nih.gov/health/health-topics/topics/hf/
©2012 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
















