Report says drug-resistant bacteria are common killers
For the first time, the U.S. government is estimating how many people die from drug-resistant bacteria each year—more than 23,000, or about as many as those killed annually by flu.
The Centers for Disease Control and Prevention released the number Monday to spotlight the growing threat of germs that are hard to treat because they've become resistant to drugs.
Finally estimating the problem sends "a very powerful message," said Dr. Helen Boucher, a Tufts University expert and spokeswoman for the Infectious Diseases Society of America. "We're facing a catastrophe."
Antibiotics like penicillin and streptomycin first became widely available in the 1940s, and today dozens are used to kill or suppress the bacteria behind illnesses ranging from strep throat to the plague. The drugs are considered one of the greatest advances in the history of medicine, and have saved countless lives.
But as decades passed, some antibiotics stopped working against the bugs they previously vanquished. Experts say their overuse and misuse have helped make them less effective.
In a new report, the CDC tallied the toll of the 17 most worrisome drug-resistant bacteria. The result: Each year, more than 2 million people develop serious infections and at least 23,000 die.
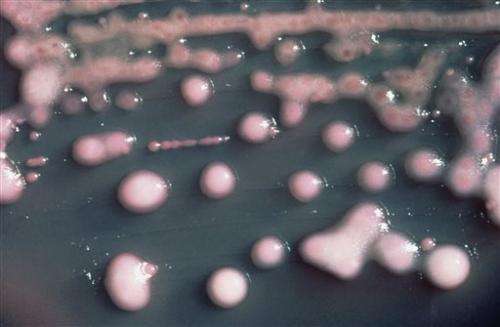
Of those, the staph infection MRSA, or methicillin-resistant Staphylococcus aureus, kills about 11,000, and a new superbug kills about 600. That bacteria withstand treatment with antibiotics called carbapenems—considered one of the last lines of defense against hard-to-treat bugs.
Germs like those have prompted health officials to warn that if the situation gets much worse, it could make doctors reluctant to do surgery or treat cancer patients if antibiotics won't protect their patients from getting infections.
"If we're not careful, the medicine chest will be empty" when doctors need infection-fighting drugs, said CDC Director Dr. Tom Frieden.
It's not clear that the problem is uniformly growing worse for all bugs. Some research suggests, for example, that MRSA rates may have plateaued and a separate CDC report released Monday in JAMA Internal Medicine found that serious MRSA infections declined 30 percent between 2005 and 2011.
MRSA bacteria have been the target of many hospital infection control efforts. These germs often live without symptoms on the skin, but also can cause skin or tissue infections, and become more dangerous when they enter the bloodstream.
Serious, invasive MRSA declined in all settings for a total of 80,461 infections in 2011, the journal report found. Most were linked with health care in people who'd recently been hospitalized or received other medical treatment. But for the first time, the more than 16,000 infections picked up in community settings outnumbered the 14,000 infections that began in the hospital.
A 2005-2010 study in the same journal suggests that pig manure might be a cause of some mostly less serious MRSA infections in people living near fertilized farm fields.
The study is based on patients from Danville, Pennsylvania.-based Geisinger Health System. It offers only circumstantial evidence, but the authors said the MRSA link is plausible because antibiotics are widely used on pig farms and other livestock operations to enhance animal growth, and the drugs are found in pig manure.
The study involved nearly 3,000 MRSA cases, about half of them not linked with health-care. The authors estimated that living near pig manure-fertilized fields may have accounted for about 11 percent of MRSA not linked with health care.
But how the germs might spread from pig manure to people with no close animal contact is uncertain, the study authors said. Close contact with an infected person or sharing personal items used by an infected person is the usual way MRSA spreads.
Dr. William Schaffner, a Vanderbilt University infectious disease specialist, called the report "very provocative" but inconclusive.
Asked generally about antibiotic use in farm animals, the CDC's Frieden said it's an important problem, but he added, "Right now the most acute problem is in hospitals and the most resistant organisms are in hospitals."
© 2013 The Associated Press. All rights reserved.















