For stroke patients, hospital bed position is delicate balancing act
During the first 24 hours after a stroke, attention to detail —such as hospital bed positioning—is critical to patient outcomes.
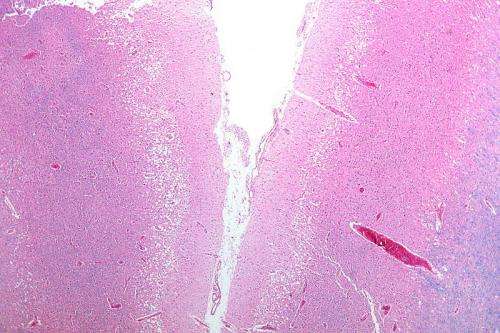
Most strokes are caused by blood clots that block blood flow to the brain. Sitting upright can harm the patient because it decreases blood flow and oxygen to the brain just when the brain needs more blood.
Thus, it's reasonable to keep patients lying flat or as nearly flat as possible, according to a report in the journal MedLink Neurology by Loyola University Medical Center neurologist Murray Flaster, MD, PhD and colleagues.
But strokes also can increase intracranial pressure (brain swelling) that can damage the brain. Sitting upright helps improve blood drainage and reduce intracranial pressure—but at a cost of reduced blood flow to the brain.
"There are few data to guide decision making in this difficult situation," Flaster and colleagues write.
Further complicating stroke care, some patients have orthopnea (difficulty breathing while lying flat). In such patients, the head of the bed should be kept at the lowest elevation the patient can tolerate.
Finally, frequent changes in body position, regardless of head position, may help patients tolerate lying flat, while also minimizing the risk of bed sores, the Loyola neurologists write.
Bed position is among the complex issues that Flaster and colleagues address in their article, which summarizes the latest research on caring for ischemic stroke patients. (Most strokes are ischemic, meaning they are caused by blood clots.)
"The period immediately following an acute ischemic stroke is a time of significant risk," the Loyola neurologists write. "Meticulous attention to the care of the stroke patient during this time can prevent further neurologic injury and minimize common complications, optimizing the chance of functional recovery."
The authors discuss stroke-care issues that can affect outcomes. For example, there is considerable evidence of a link between hyperglycemia (high blood sugar) and poor outcomes after stroke. The authors recommend strict blood sugar control, using frequent finger-stick glucose checks and aggressive insulin treatment, regardless of whether the patient has a known history of diabetes.
For each 1 degree C increase in the body temperature of a stroke patient, the risk of death or severe disability more than doubles. Therapeutic cooling has been shown to help cardiac arrest patients, and clinical trials are underway to determine whether such cooling could also help stroke patients. Until those trials are completed, the goal should be to keep normal temperatures (between 95.9 and 99.5 degrees F).
The authors discuss many other issues in stroke care, including blood pressure management; blood volume; statin therapy; management of complications such as pneumonia and sepsis; heart attack and other cardiac problems; blood clots; infection; malnutrition and aspiration; brain swelling; seizures; recurrent stroke; and brain hemorrhages.
Studies have shown that hospital units that specialize in stroke care decrease mortality, increase the likelihood of being discharged to home and improve functional status and quality of life.















