Innovation in neurosurgery
As medical students, we don't get much intra-curricular exposure to surgery. Then there is the neurophobia, a chronic condition whose main symptom is the inability to apply knowledge of neuroscience to clinical situations. A phenomenon literature suggests is fairly common, and experience tells me is already afflicting my student cohort. As we waited to enter our exams a few months ago, one person voiced what we we'd all been thinking: "I really hope there's not much brain in this one!" Perhaps as a result of this neurophobia and limited insight into surgical careers, the relatively small specialty of neurosurgery seems to be shrouded in a certain level of mystery for many medical students.
Last week, the SBNS – one of the world's oldest neurological societies – held their bi-annual meeting in the city of York, hosted by surgeons from my teaching hospital and Neurosurgical Unit (NSU), the Hull Royal Infirmary (HRI). As their first ever 'press pass' delegate, I was fortunate to attend SBNS York 2015. I will try to describe my experience and outline some of the main areas of discussion.
Pesky Prions
The conference began by discussing variant Creutzfeldt-Jakob disease (vCJD), occasionally referred to in the media as the human form of mad cow disease due to its link with the consumption of beef infected by Bovine spongiform encephalopathy (BSE). The human prion disease vCJD is an incurable, fatal, neurodegenerative disorder. Fortunately, it is also very rare.
Those born after 1996 in the UK are said to be at 'near zero risk for vCJD' thanks to the successful containment of BSE in cattle at that time; but this poses a neurosurgical dilemma. Guidelines recommend separate sets of surgical instruments for post-96 and pre-97 patients, but it can be difficult to assemble a full post-96 set. In these cases, the Chair asked, does duty of candour oblige us to inform patients that we are using pre-97 kit? There was a varied audience response to this ethical question, with one delegate pointing out that he'd probably have bigger things to worry about if he were about to have brain surgery. Are some risks so small that going into them constitutes an unnecessary and potentially damaging disclosure? At my medical school, we call these Theme C questions, which fall under the remit of Health & Society and Professionalism, but we very rarely engage in the kind of spirited debate that was happening here. I think there is a lot of conference behaviour that would be well suited in medical education.
The debate moved on to the paramount issue: how do we minimise the risk of vCJD transmission in neurosurgery? Single-use surgical instruments seemed to be the most sensible option, certainly for procedures in those born after '96 who have previously had surgery with pre-97 kit. One delegate suggested money might be better spent on developing a suitable detergent, but repeated use might damage reusable instruments, and we would have to be certain that the process could be run safely and effectively across all NSUs. The question that at first seemed so simple was fraught with practical considerations, financial constraints, and concerns over sustainability. It also seemed to be an example of how current guidance does not match up with current practical feasibility.
Innovation in Hull
I was very proud that this conference was being hosted by my teaching hospital, and even more so that their innovative practice featured in many presentations. HRI NSU is the 18th largest in the country, but has become the 3rd busiest for spinal elective cases, primarily through their novel collaboration with physiotherapists.
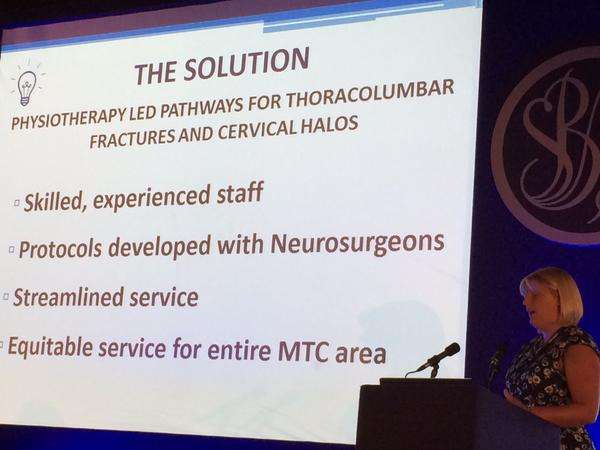
Sally Fenton, Clinical Lead in Physiotherapy, explained how they have streamlined the management of spinal fracture patients using a new model of physiotherapy-led follow-up. Their innovative pathway has been extremely effective, with no adverse clinical outcomes, and a 332% increase in activity over 5 years. Physiotherapist Michelle Naylor went on to outline the success of their physiotherapy-led telephone follow-up service for patients after spinal surgery where an impressive 75% of patients were discharged directly to the GP without further need for consultant follow-up. The benefits of these physiotherapy-led services seem to be in reducing consultant work-load, thereby freeing up more time for clinics and surgeries, reducing waiting lists, and improving patient communication by providing them with a single point of contact within the service. Similarly, the novel nurse-practitioner-led cervical fracture service presented by S. Newton provides an open access service at all times if patients have any problems.
"If you ladies want to come work in Cambridge, you'd be very welcome!" announced a voice from the audience following the presentations. "We've already offered them a job in Oxford," replied another. Fortunately, I think they'll all still be sticking with us at HRI and continuing their exceptional work.
Globetrotting
"I think we need a group of surgeons who are globe trotters, who can practice in different countries without these artificial barriers in place," said Mr Tom Cadoux-Hudson from the John Radcliffe Royal Infirmary in Oxford, as international neurosurgeons discussed the possibility of a cohesive global process of training and examination. Maybe an SGNS (Society of Global Neurological Surgeons) is some way off, but I particularly enjoyed hearing about how surgeons are collaborating in different countries. Dr Laxminarayan Tripathy, Chief Neurosurgeon and Vice President of the private Medica Superspecialty Hospital, whose passion for teaching was obvious, told us about the training of Nigerian surgeons in Kolkata, India. I was pleasantly surprised to see that his presentation also featured a friend of mine, Tom Robbins, President of our school's Surgical Society.
Tom's passion for neurosurgery was inspired by the host of this conference Mr Bruce Mathew, a senior consultant neurosurgeon at HRI, and it was through the help of Mr Mathew that Tom's elective attachment with Dr Tripathy became a reality. Talking of his time in Kolkata, Tom told me: "Medica Superspecialty hospital was set in the Mukandapur district on the outskirts of Kolkata and was resourced as well as any NHS equivalent hospital. I witnessed the use of brain lab and CUSA for accurate removal and debulking of various brain tumours. There were clean, air-conditioned clinic rooms and swish new wards facilitating excellent pre-surgical and post-surgical care. Such facilities are commonplace back in the UK but what made all of this seem extra special to me was the moment I walked out of the hospital doors. Many of the roads were flooded and crumbling, as it was the height of the monsoon season, the traffic was stationary and there were frequent power outages. Yet despite this seemingly saturated and under-resourced civic infrastructure, Medica Hospital was still flourishing and providing cutting edge care to patients against the odds, much to the credit of Dr Tripathy. My impression of my time spent working in Medica in Kolkata would perhaps be: despite the superficial appearance of disorder there is an underlying thread of intense productivity and so long as you didn't try to resist this chaos, you could get things done too."
Reassembled, Slightly Askew
I feel that no scientific conference is complete without an arts contribution. At SBNS York 2015, this contribution came from Shannon Yee with her spectacular immersive audio experience "Reassembled, Slightly Askew."

Delegates were invited to lie down on patient beds, put on eye masks and headphones, and listen to this incredible piece of theatre, created to depict Shannon's journey as a patient descending into a coma from a subdural empyema, undergoing surgery, and her subsequent rehabilitation with an acquired brain injury.
"It is normal to feel a bit disoriented, so don't worry if you need some time to yourself afterwards," said Shannon as I got ready to put on the headphones. The whole experience was a bit unnerving. It made me feel like I was inside someone else's head with little control of my surroundings and therefore quite vulnerable – how any patient must feel in a hospital, especially when they can't comprehend what is happening to them. I think high-quality art projects like this provide an excellent way in to understanding the patient experience. Shannon's project definitely falls under the heading Innovation in Neurosurgery and was a refreshing addition to the conference.
Feeling introspective, I heeded Shannon's advice and went outside for a few minutes in the Yorkshire sunshine.
Closing Comments
"I think the success of a meeting can be measured by its delegates' willingness to provide both positive and negative comment," said Richard Kerr. By the standard set out in the president's closing remarks, the meeting was a great success. Throughout the event, people openly questioned each other and weren't afraid to disagree, but there was a consistently friendly atmosphere in the room. I'd even go as far as to say it was cosy.
Hopefully, fellow medical students will start to see neuro as less of a mystery and more of an exciting field of study and accessible area of surgical practice. I also hope that all students, from their very first day at medical school, will feel able to take the time to go to conferences in any field that interests them. I think it is beneficial to pursue what you are passionate about at an early stage, even if that passion may change or evolve in the future.
The SBNS conference was a pleasure to attend. I met some wonderful people, witnessed the presentation of world-class research, and now know how to correctly pronounce ependymoma. What more could I ask for!
This story is republished courtesy of PLOS Blogs: blogs.plos.org.

















