New study suggests hallucinations, alone, do not predict onset of schizophrenia
Despite decades of study, schizophrenia has remained stubbornly difficult to diagnose in its earliest stage - between the appearance of symptoms and the development of the disorder. Now, a new analysis led by researchers at the UNC School of Medicine and the Renaissance Computing Institute (RENCI) identified illogical thoughts as most predictive of schizophrenia risk. Surprisingly, perceptual disturbances - the forerunners of hallucinations - are not predictive, even though full-blown hallucinations are common features of schizophrenia. The results were published online today in the journal Schizophrenia Research.
"The earlier people are identified and receive treatment when they develop schizophrenia, the better their prognosis," said Diana Perkins, MD, a clinician and professor of psychiatry at the UNC School of Medicine and one of the study's first authors. "If we can identify people at high risk for psychosis we can then develop interventions to prevent the development of schizophrenia and the functional declines associated with it."
Schizophrenia is a chronic mental illness that affects more than 3 million people in the United States. It typically emerges during late adolescence and early adulthood, and remains a chronic and disabling disorder for most patients. Psychosis, which more than 6 million Americans experience, refers to a group of symptoms, including paranoia, delusions (false beliefs), hallucinations, and disorganization of thought and behavior. Psychosis always occurs in schizophrenia, but can also occur in people with bipolar disorder or other medical conditions.
Early warning signs of schizophrenia include mild psychosis-like symptoms. However, only about 15-20 percent of people who have these mild psychosis-like symptoms actually develop schizophrenia or other disorders with full-blown psychosis. Current diagnostic criteria for attenuated psychosis include having at least one of the following: illogical thoughts, disorganized thoughts, or perceptual disturbances of sufficient frequency and severity to impact function.
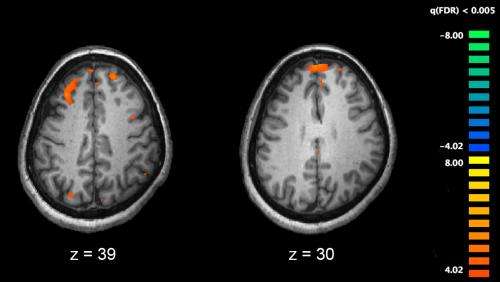
To help clinicians know where to draw the line, Perkins and Jeffries examined what symptoms were most predictive of psychosis over a two-year follow-up period in a cohort of 296 individuals at high-risk for psychosis because of experiencing attenuated psychosis symptoms. The analysis revealed that suspiciousness and unusual thought content were the most predictive, and that difficulty with focus or concentration and reduced ideational richness further enhanced psychosis risk prediction.
Identification of the most informative symptoms was performed with "stringent randomization tests," according to the other first author, Clark D. Jeffries, PhD, a scientist at RENCI. That means the same classifier algorithm was applied to the true data as well as 1000 random permutations of the data that mixed patients who did and did not progress to frank psychosis.
Importantly, the investigators validated these findings in a new cohort of 592 people with attenuated psychosis symptoms, confirming the findings. Suspiciousness and unusual thought content include a "feeling of being watched," or "it seeming like others are talking about" the person but knowing that this "can't really be true," or fixating on coincidences that aren't actually connected, or finding "signs" in certain experiences or having a distorted sense of time.
Difficulty with focus and concentration refers to problems with distractibility and short-term memory. Reduced ideational richness typically refers to difficulty following conversations or engaging in abstract thinking.
Somewhat surprisingly, perceptual disturbances - seeing shadows or hearing knocking noises with a sense that these experiences are "not real," - while superficially similar to hallucinations were not predictive of psychosis. Although such symptoms were common in those who developed psychosis, they were equally common in those who did not develop psychosis.
"In terms of assessing psychosis risk, I think this study shows we need to be emphasizing the person's thought process, and appreciate that perceptual disturbances may not be a specific early warning sign," Perkins said. "I think that will affect how we develop our diagnostic system in the future for people who are at high risk for psychosis."















