New study indicates why children are likelier to develop food allergies

An estimated 15 million Americans suffer from food allergies, many of them children. These are non-trivial concerns, as food allergy or intolerance can cause symptoms ranging from a harmless skin rash to a potentially lethal anaphylactic shock. The good news is that many affected children outgrow their allergy, presumably as the immune system learns to tolerate food initially mistaken as "foreign".
A new study published in the January 28, 2016, online issue of Science by La Jolla Institute for Allergy and Immunology (LJI) researcher Charles Surh, Ph.D., may explain how food tolerance emerges over time in normal individuals.
Coupling molecular approaches with a long-forgotten model of "antigen-free" mice, the study is the first to demonstrate that consumption of a normal diet stimulates cells in the gut that suppress rejection of food by the immune system. Knowing this could explain why children, who have more limited exposure to novel foods than adults, are more susceptible to food allergies.
"The immune system evolved to protect us from things that are not ourselves, like viruses or pathogens, yet we consume nutrients, which are themselves foreign," says Surh, an adjunct professor in LJI's Division of Developmental Immunology. "Our work shows food tolerance is acquired and involves specific populations of T cells that develop following its consumption. Without them, we would mount a strong immune response to macromolecules contained in food."
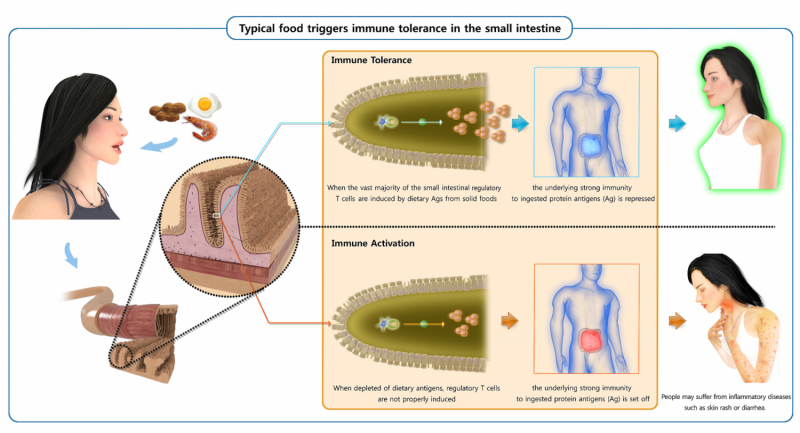
Like pathogens, food displays macromolecular markers known as antigens that announce to the immune system that food is "foreign". Previous analysis of how the body distinguishes antigenic friend from foe revealed that feeding lab mice a novel test protein—for example, the egg protein ovalbumin—induced development of immunosuppressive T-regulatory, or "Treg" cells, in the gut, which then acted to block the immune response to that particular protein. What researchers didn't know was whether this happened in "real life" as young mammals—be they mouse pups or human toddlers—encountered new foods.
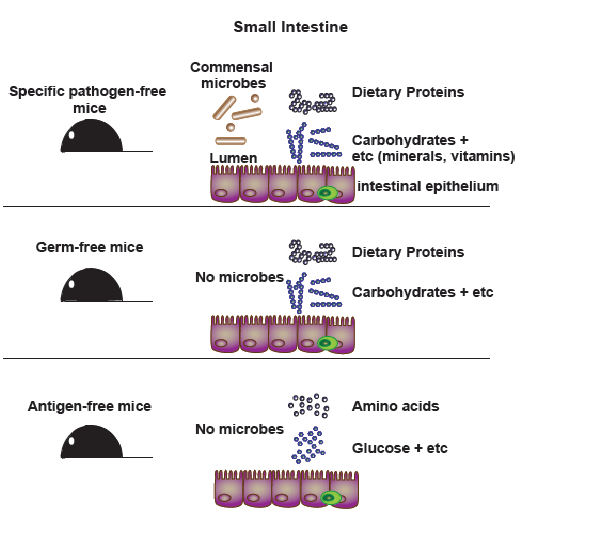
To address that question, Surh re-established "antigen-free" mouse models designed to represent an immunological blank slate. These animals were not only raised in a germ-free environment but were also fed an "elemental" diet of amino acids, the building blocks of proteins, rather than foods that contain intact proteins themselves. The mice were, in essence, immunologically naïve, because the amino acid building blocks are too small to be recognized by the immune system. These mice therefore have little or no prior contact with antigenic proteins and other macromolecules.
Using molecular marker analysis, Surh and colleagues found that antigen-free mice were depleted of Tregs in the small intestine whereas a large number of these Tregs were present in germ-free counterparts fed a "normal" protein diet. That difference alone suggested that proteins contained in food stimulate Treg development. It also hinted that Tregs present in the gut of normal mice might suppress a potentially disastrous immune response to those proteins.
Surh says antigen-free mice are not new, just forgotten, as their prototypes were developed over 30 years ago to study nutrition. "We brought them back because we're no longer in the dark ages: We know a lot more about immunology!" he says. "Decades ago, researchers could monitor changes in lymphocyte numbers but couldn't distinguish between cell types like we can now."
The researchers took full advantage of these technical advances to also demonstrate that food and the beneficial bacteria in the intestine generate molecularly distinct populations of Tregs. Hence, germ-free mice only possess the food-dependent Treg, but not the Tregs that are induced by the healthy microbes. Intriguingly, germ-free mice are known to be highly susceptible to allergies. Hence, Surh hypothesizes that the presence of both food- and microbe-induced populations of Tregs is required to prevent allergic symptoms.
Finally, the team revealed what happens when immune cells fail to ignore harmless antigens. To do so, they transferred "reporter" T cells designed to serve as a read-out for an immune reaction into antigen-free mice and then fed mice a test protein they had never encountered (the lab stand-by, ovalbumin). Those mice mounted a massive immune reaction—what Surh calls the default response— to ovalbumin relative to germ-free mice fed a normal diet.
This dramatically inappropriate reaction to a nutrient resembled the immunological storm aroused by harmful microbes. Surh's group concludes that it occurred because the antigen-free mice had not readied a population of immunosuppressive Tregs that would normally be primed to dampen an inflammatory response to food.
By extension, the new work could explain why children, who have more limited exposure to different types of novel nutritious macromolecules (that is, food) than adults, are more susceptible to food allergies. It also suggests what happens on a cellular basis as some outgrow it: namely, they may be expanding their repertoire of Tregs that recognize new foods as "safe".
Those issues continue to interest Surh, who in addition to his position at LJI is a director and professor in the Academy of Immunology and Microbiology (AIM) at the Institute for Basic Science (IBS) in Pohang, in Korea. "We are now examining the cellular and molecular details of how the 'default' strong T cell response to food is regulated," he says. "In this context, we plan to pay particular attention to certain foods, such as peanut, egg and other foods that cause food allergy."
More information: "Dietary antigens limit mucosal immunity by inducing regulatory T cells in the small intestine," by K.S. Kim; S.-W. Hong et al. DOI: 10.1126/science.aac5560















