The enduring need for cancer treatment
Danielle Rodin is a Radiation Oncology Resident at the University of Toronto and co-founded the group GlobalRT, which is a group of young professionals dedicated to improving the availability and accessibility of radiation therapy resources for cancer patients in low-resource settings. Daniel Smith is a recent Medical Physics PhD graduate from the University of Texas MD Anderson Cancer Center, and heads the physics section of GlobalRT. They share their thoughts on expanding equitable treatment options globally, in time for World Cancer Day.
Global health involves the provision for populations of what has been termed "health security". When the World Health Organization was formed in 1948, this term referred to acute public health threats, such as those due to epidemics of infectious disease, or to military actions. However, over 60% of the world's deaths are now due to non-communicable diseases (NCDs), including heart disease, cancer, diabetes, and chronic respiratory diseases. Public health interventions are widely recognized to play a major role in controlling morbidity and mortality related to these conditions.
In 2011, the United Nations General Assembly met on a health issue for only the second time in its history and declared that NCDs "constitute one of the major challenges for development in the twenty-first century, which undermines social and economic development throughout the world and threatens the achievement of internationally agreed development goals". International targets have been set to address this modern threat to health security, but whether they can be achieved depends on a number of critical next steps.
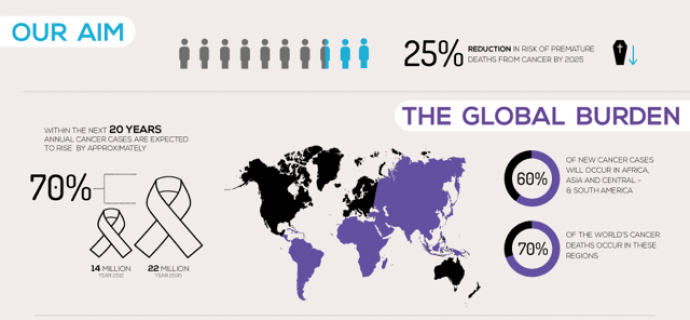
In 2012, 14.1 million new cancer cases and 8.2 million cancer deaths were reported. These figures are expected to rise dramatically by 2030 to 24.6 million new cases and 13 million deaths. While cancer is the leading cause of early death worldwide (and second leading cause of death overall), the majority of these deaths disproportionately occur in low-and-middle income countries (LMICs). This disparity reflects the lack of adequate cancer services in LMICs across the cancer care continuum, from prevention and early detection to palliative care.
For World Cancer Day 2015, this blog focused on prevention. This is an essential measure in cancer control, since more than 30% of cancers are preventable through tobacco control, healthy diet and exercise, reduced sun exposure, and vaccination.
However, the full effects of cancer prevention will not be realised for decades and, despite our best efforts, prevention sometimes fails. Further, two-thirds of cancer cases cannot be prevented.
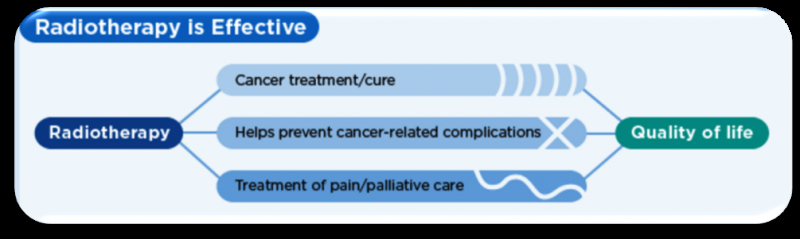
Cancer is typically treated using a multimodal approach that includes surgery, radiation, and drug therapy. Half of all cancer patients require radiation as part of their treatment for either curative purposes or to control symptoms of the disease such as pain, bleeding, and shortness of breath (Figure).
However, despite this demonstrable need, over 90% of the population in low-income countries lacks access to radiotherapy, and although LMICs account for 80% of the global cancer burden, they possess only 5% of the world's radiotherapy resources. In sub-Saharan Africa, most countries almost completely lack access to radiotherapy.
The geographic disparity in the availability of radiotherapy is perpetuated by unsubstantiated beliefs that it is too costly or impractical to implement in low-resource settings. However, this view fails to account for the staggering worldwide economic burden of inadequately treated cancer, estimated to be $2 trillion in 2010. This economic burden is driven primarily by expenditures on healthcare and by reductions in labour productivity due to disability and premature death. The adverse economic impact of inadequately treated cancer on individual families and communities is enormous, as cancer patients without access to treatment disproportionately leave the labour force, resulting in income loss for their families that reverberates through generations.
In 2013, the Global Task Force on Radiotherapy for Cancer Control (GTFRCC), an international collaborative effort between oncologists, physicists, economists, industry and global health experts, was established to quantify the investment needed to achieve global equity in access by 2035. The GTFRCC later became part of the Lancet Cancer Campaign as The Lancet Oncology Commission on Global Radiotherapy. This Commission found that investing in radiotherapy not only saves and prolongs lives, but also boosts economies. Applying a realistic 20-year radiotherapy scale-up plan in LMICs, investing in radiotherapy would result in a savings of 27 million life-years and a net economic benefit of up to $365 billion.
Based on the GTFRCC findings, the task force issued a call to action and established a set of global targets:
- Incorporate radiotherapy into population-based cancer control plans in 80% of countries by 2020.
- Increase the 2015 radiotherapy treatment capacity 25% by 2025, including the establishment of at least one cancer centre in each LMIC by 2020.
- Train 7500 radiation oncologists, 20000 radiation technologists, and 6000 medical physicists in LMICs by 2025.
- Invest $46 billion by 2025 to establish radiotherapy infrastructure and training in LMICs.
- Include radiotherapy services as part of the UHC plans for universal health coverage in 80% of LMICs by 2020.
The feasibility of this dramatic expansion of radiotherapy in LMICs is already being demonstrated in India, Bangladesh, Zimbabwe, and Brazil. Further success in expanding radiotherapy capacity will depend on the presence of enabling environments and coordinated efforts among institutions, such as the World Health Organization, the International Atomic Energy Agency, and the Union for International Cancer Control. It will also require the support of multilateral development agencies, civil society, professional associations, and the private sector. Innovations in technology, communication, and financing are underway and are critical to overcome many of the practical barriers that limit access to radiotherapy. However, political will is also needed to make this happen. GlobalRT was created by the GTFRCC Young Leaders Program in order to stimulate engagement in this project. Over the course of eighteen months, it has engaged over 3000 users around the world in advocacy for improved access to radiotherapy treatment and cancer care.
The GFTRCC has generated evidence to support advocacy for the expansion of radiotherapy in LMICs. However, scientific evidence alone does not result in major health systems-level change. The work of the GTFRCC has helped to galvanize other important factors necessary to translate evidence into policy. With transformational leadership, medical community action, public awareness, and grassroots mobilisation, 2016 could be a watershed year in the journey toward global health equity in radiotherapy for cancer.
This story is republished courtesy of PLOS Blogs: blogs.plos.org.














