Adapting the transtheoretical model of behavior change to understand PrEP engagement
One of the most groundbreaking HIV prevention strategies for HIV-negative gay and bisexual men (GBM) is a once-daily pill called pre-exposure prophylaxis (PrEP), which is up to 99% effective in the prevention of HIV infection. Despite this high rate of effectiveness, there is a dramatic gap between the number of GBM who could benefit from PrEP for HIV prevention and those who are using it. Two recently published papers from CHEST have helped understand the reasons for this gap using data from One Thousand Strong, a longitudinal study following a national cohort of over one thousand HIV-negative GBM for three years.
In the first paper, published in Social Science and Medicine, the authors identified one potential reason for this gap. Based on this, the authors then sought to empirically look at movement along the full continuum of PrEP engagement in a subsequent paper, published in JAIDS: Journal of Acquired Immune Deficiency Syndrome—this paper was the first to examine the PrEP cascade using a national sample of GBM in the U.S.
The first paper was led by Dr. Jonathon Rendina, Assistant Professor of Psychology at Hunter College, CUNY and Director of Quantitative Methods at CHEST. He explained the rationale behind the study: "Research for years has shown that most gay and bisexual men are willing to take PrEP in an idealized situation where it's provided for free and just sort of shows up at your doorstep, but uptake has been surprisingly low. We thought that men may be willing to take it but might not see themselves as needing to take it right now and also that, even after that, part of the problem may be developing and executing a plan to go through all of the actual steps required to get on PrEP." The findings confirmed that there is a distinction between hypothetical willingness to take PrEP and actual intentions to begin a PrEP regimen—only a fraction (28%) of GBM who reported they might be willing to take PrEP also reported they actually planned to begin it. Additionally, results showed that men who were aware of PrEP's high level of effectiveness and those men who saw themselves as good candidates for PrEP were more likely to intend to take PrEP. These results highlighted clear targets for interventions aiming to facilitate PrEP engagement—namely, education about PrEP's efficacy and who can benefit from it the most.
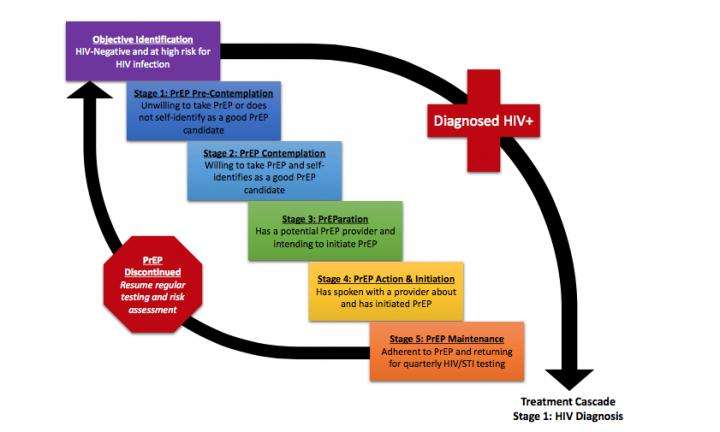
The second paper was led by Dr. Jeffrey Parsons, Distinguished Professor of Psychology at Hunter College, CUNY and Director of CHEST. He noted that, "The first study helped us to understand one of the drop?off points where we lose people in the continuum, but we wanted to understand the full range of steps involved in PrEP engagement from beginning to think about it to getting on it and staying on it." To do that, CHEST researchers analyzed data from 995 of the One Thousand Strong participants who completed a 12?month follow up survey—they based their proposed cascade on the HIV Care Continuum (used to show engagement in care for HIV?positive individuals) and some prior work on PrEP engagement. Dr. Parsons described, "We wanted the cascade to have clear intervention techniques that could be used at each step, so we based it on the Transtheoretical Model (Stages of Change), which has been used for decades to guide effective interventions for both HIV prevention and treatment. The five stages of the "Motivational PrEP Cascade" were developed by grouping different steps in the process of PrEP engagement into stages that correspond with stages of change within the Transtheoretical Model. Then the researchers examined empirical data for how many men in One Thousand Strong had made it through each of the stages.
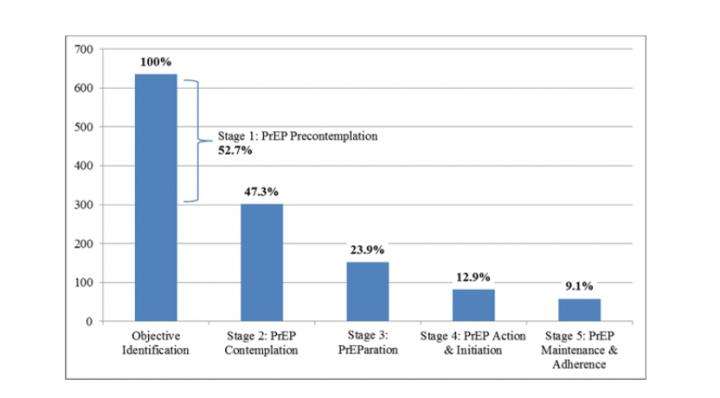
Dr. Parsons and his team first began by determining how many men would qualify as candidates for PrEP based on CDC criteria—this objective identification ensures that men who don't need PrEP aren't counted toward the numbers at each stage of progression. In total, roughly two?thirds of men in this sample met objective criteria suggesting they could benefit from PrEP. Of the 642 GBM that met these criteria, fewer than 1 in 10 self-reported being on PrEP and adherent to guidelines about adherence and medical monitoring.
Taken together, these results highlight the need for a comprehensive strategy beneficial to both health providers and their patients to facilitate conversations about whether PrEP is an appropriate prevention strategy for them. Dr. Rendina noted that, "These data showed that the majority of GBM might be good candidates for PrEP based on CDC criteria and yet we are missing out on opportunities to reduce new HIV infections at every point along the path of PrEP engagement, with particularly high drop off in the beginning stages." Both of the studies pointed to the fact that not believing you are an appropriate candidate for PrEP and not having a plan to get on PrEP are two of the biggest points at which people are lost along this continuum. Dr. Parsons pointed out that, "We need to address these early phases first or we will never have uptake of PrEP among GBM. Researchers and providers are spending a lot of time focusing on concerns about PrEP adherence, but adherence is irrelevant if nobody is taking PrEP in the first place." Given the large drop off at these early points, research suggests that straightforward education about PrEP and HIV risk coupled with conversations with providers about the benefits and drawbacks of starting PrEP has the potential to make a dramatic shift in the cascade. These findings also suggest that one way to help increase uptake and ultimately adherence is for providers to meet potential PrEP candidates where they are and tailor PrEP?related discussions based on where they fall along these stages.
















