Urinary test can detect bladder cancer, reduce discomfort and save money
Urinary bladder cancer is one of the most expensive cancer forms for the public health service. Norwegian researchers are developing a test that will benefit both the system and the patients. They plan to launch a candidate test by the end of 2017.
Patients who have been through surgery for urinary bladder cancer must go through several expensive and somewhat unpleasant controls to check for recurrence. Norwegian researchers are developing a urinary test that can save money and discomfort, and plan to launch a candidate test by the end of 2017.
Cancer in the urinary bladder results in approximately 170,000 deaths internationally each year, and it is the fourth most common type of cancer in men in the United States. In Norway, more than 900 men and some 350 Norwegian women develop cancer in the urinary bladder each year.
The standard treatment is to remove the cancer-affected areas inside the bladder wall, and the results are generally quite good. At the beginning of 2010, almost 11,000 men and women diagnosed with bladder cancer were alive in Norway, and more than half of them had lived more than five years with the diagnosis – and one third had lived for more than ten years. These are quite good statistics compared to several other types of cancer, which are both more common and have higher mortality rates.
But even if urinary bladder cancer is not the most common type of cancer, it is one of the most expensive for healthcare systems in developed countries. The main reason is that the follow-up of patients after surgery is very demanding, according to Professor and Group Leader Guro E. Lind at Oslo University Hospital.
"The cancer relapses after surgery in up to 70 percent of the patients, so each and every one must be closely monitored for several years. The most common follow-up is by cystoscopy, which is carried out with a small instrument, shaped like a thin tube, inserted through the urethra and into the urinary bladder. The cystoscope is equipped with a small camera that allows for a visual inspection of the inside of the bladder, and the urologist can use special tools to take samples of areas that look suspicious," Lind explains to Titan.uio.no.
Looking for "tags" on the cancer cells
Each patient has to go through such checkups many times: The average is 15 to 20 cystoscopies spread over several years after surgery.
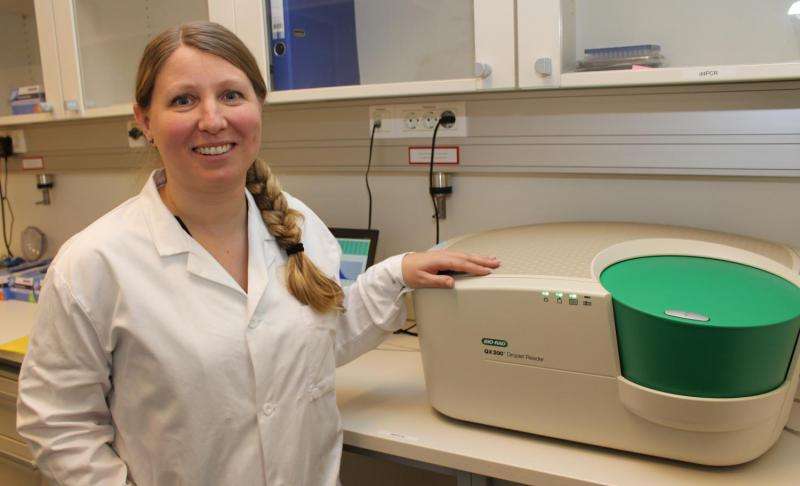
"These checkups are both costly for the society and uncomfortable for the patient. Therefore, we want to develop a urine-based test that can replace many of the cystoscopies," says Guro Lind. She is heading the Epigenetics Group at Oslo University Hospital, where researchers already have come a long way in this work. Their vision is to find a "tag" that exists only in the urine of people with bladder cancer, and which can be identified in a relatively simple way.
"The plan is to have a solidly documented proposal for such a tag, or rather a small set of tags, by the end of 2017. By then, we should have come far enough for Inven2 to start looking for business partners who can develop our tags into a commercially viable test for bladder cancer," Lind says. Inven2 is the University of Oslo's and Oslo University Hospital's joint company for innovation, and the largest contributor in Norway within the field of commercialization of research.
Inven2 has great faith in the project and foresees that a urine-based test can meet a very large medical need with significant commercial interest.
"Consequently, the project is highly prioritized by us. The preliminary data are promising, and although this is a highly competitive field, our hope is that we shall be able to develop a competitive product. We have a very good cooperation with the inventors/researchers at the OUS, who belong to a group with solid experience from innovation in molecular diagnostics," says Inven2's Technology Strategy Manager Mohammed Amarzguioui.
Simple test, complicated development
Guro Lind envisions that the test itself can be relatively simple. The basis for the whole idea is that urine in healthy people contains normal cells from the inside of the urinary bladder, but in cancer patients, the urine also contains cells from the cancerous tumour.
It is quite easy for skilled pathologists to detect cancer cells in urine from advanced tumours using an ordinary microscope, but this technique is less effective in detecting the early stages of cancer.
Fortunately, recent advances in epigenetics, with studies of methylation and the development of what is called digital PCR technology, has created new opportunities:
Epigenetics is the study of how heritable traits in organisms can change without the actual DNA code being changed.
Methylation is the process behind epigenetic changes: It occurs when a small molecule – a methyl group – is attached to a DNA strand and acts as part of a switch that can turn genes "on" or "off."
Digital PCR technology can be used to detect rare molecules, such as specific methylated DNA sequences in an ocean of unmethylated variants.
"We know from previous research that methylation occurs frequently in cancer – but it also occurs early in the cancer development. In malignant tumours, we can find several hundred or up to a thousand regions that have aberrant methylations. Identifying the methylation changes that only occur in bladder cancer and never in healthy bladders is however challenging," Lind explains.
"This has been like looking for the famous needle in the haystack. But now, we are finally in the process of identifying a small number of promising methylation aberrations that may be used as precise tags."
Hunting high and low
Professor Lind adds that the researchers have hunted "high and low" in the human DNA, to find the best epigenetic tags for bladder cancer.
"It is fascinating that most of the tags we have ended up with occur in parts of the genetic material that currently has no known function. At the beginning of the project, we looked for methylation changes in genes that had something to do with cancer development. Although this gave us relatively good tags, we soon realized that we had to expand the search to reach our goal. The best tags we have found appear to be "stowaways" that have no link to known cancer genes," she says.
All these tags have been detected by DNA methylome sequencing. But when Guro Lind and colleagues have a complete set of such methylation "tags," they will use the already mentioned digital PCR technology – which is both fast, precise and with reasonable costs – to detect the bladder cancer from urine samples.
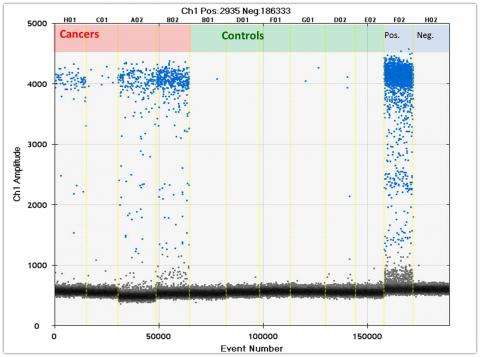
"Urine samples from patients with cancer normally contain a lot of normal cells, but only a few cancer cells – which in many ways will "drown" in the signals from the normal cells. What's cool with digital PCR is that we can convert each sample into thousands of small droplets by pushing the urine through a special type of oil. In this way, the signals from the cancer cells and normal cells become spread out between different droplets, so that each small signal can be read accurately," Guro Lind explains.
This technology ensures that the strong signal from the normal cells will no longer drown the weak signal from the cancer cells, which the system automatically labels with a fluorescent dye.
"We are developing an algorithm that separates healthy and cancerous urine samples simply by counting the number of droplets with a clear positive signal," explains Lind, while demonstrating a digital PCR machine.
She further explains: "We are developing a technique that doesn't depend on expensive DNA sequencing. The digital PCR machine just looks out for the tags we have identified, and this is a much faster and cheaper process. The machine may look a lot like Grandma's old foot bath, but the inside of the machine is much more advanced!"
Saving health care a lot of money
The aim of the researchers at Oslo University Hospital is that the new test should offer patients after-surgery controls that are as safe and accurate as the current procedure, but in a way that reduces the number of uncomfortable cystoscopies. In addition, they hope that the test can reduce the expenses for society as a whole.
The large number of follow-up investigations being carried out today is namely a great economic burden on the healthcare system.
"You have to be a specialist, a highly trained urologist, to perform the many cystoscopies that are used today. If our urine-based test can replace part of these cystoscopies, urologists can spend more time on other things instead. But the test can't replace cystoscopy completely: When our test marks a positive finding, patients need to be investigated more closely with cystoscopy, explains Lind.
Urine samples by taxi three times a day
Professor Lind adds that the researchers have encountered some unexpected practical challenges during the project. It proved to be very time-consuming to collect the urine samples that was needed in the project, and Lind has great appreciation for the work done by partners Dr Rolf Wahlqvist, research nurse Anne Klara Sørbø and other colleagues at the Department of Urology at Oslo University Hospital.
This is where most bladder cancer patients in the Oslo region are being treated, and each patient that enrols in the project must agree to deliver urine samples before and after surgery and follow up samples for up to two whole years.
Urine is not the best environment for cells, and if stored too long, the cells will lyse and the DNA will be lost. Therefore, the researchers had to organize a system that allowed fresh samples to be sent by taxi three times a day from the Department of Urology on the east side of Oslo, to the research department some eight miles further to the west.
"We take turns to carry a dedicated cell phone, and the researcher on "sprint duty" have to run to the hospital's entrance every time a taxi arrives with a sample. Thereafter, he or she rushes to our laboratory to centrifuge the urine, and finally we freeze the cells to be studied later," Lind explains.
Facts on bladder cancer:
- Bladder cancer is less common in women than in men, scientists are not sure about why.
- Smoking and exposure to pollutants increase the risk of bladder cancer.
- Visible blood in the urine is the most common and often the only external symptom.
- Cancer in the urinary bladder tends to return to 70 percent of the patients - which must be operated again.
- Many women with bladder cancer come to the doctor late, because the early symptoms resemble urinary tract infections.
More information: V. L. Costa et al. Three Epigenetic Biomarkers, GDF15, TMEFF2, and VIM, Accurately Predict Bladder Cancer from DNA-Based Analyses of Urine Samples, Clinical Cancer Research (2010). DOI: 10.1158/1078-0432.CCR-10-1312
















