Scientists move closer to detecting cancer long before any symptoms appear
The quest to detect cancer before it grows deadly has taken another step forward, with new proof-of-concept data showing that a specialized blood test can spot bits of mutated DNA shed by tumors too small to be identified any other way.
The breakthrough study was presented at the annual meeting of the American Society of Clinical Oncology in Chicago, which ends Tuesday. It found that 73 percent of genetic mutations detected in the tumors of 124 advanced cancer patients were also discovered in bits of DNA floating freely in their blood.
What's more, by also sequencing the patients' immune-system white blood cells, the researchers were able to filter out mutations arising from a person's natural aging process - mutations that aren't cancerous but resemble those originating from malignant tumors.
The discoveries came from GRAIL, a San Francisco-based spin-off of DNA sequencing giant Illumina in San Diego. They validate the "high intensity" sequencing method, which involves reading targeted regions of the genome an average of 60,000 times to boost accuracy. GRAIL intends to use this technique in a study of 10,000 Americans - people with cancer and those without the disease.
"This is our feasibility study to make sure that this approach actually works," said Dr. Pedram Razavi, a medical oncologist with the Memorial Sloan Kettering Cancer Center in New York who is working with GRAIL.
Seeing a direct correlation between known cancerous tumors and mutated strands of DNA in patients' bloodstreams is an important first step in what will be a long path toward using blood tests to determine who has cancer and who doesn't, said Dr. Mark Lee, head of clinical development for GRAIL.
"This gives us more confidence as we move into larger-scale studies across different tumor types and at much larger scale," Lee said.
As the company's name implies, developing a blood test that can detect cancer so early that it's not yet visible on the X-rays and other tests used today would be Holy Grail of cancer prevention.
The theory goes that by uncovering the cancer early enough and determining how slow-growing or aggressive it might be, doctors will be able to mount a much more effective response using an ever-expanding arsenal of tailored treatments. The latest strategies include the field of immunotherapy, where drugs customized for different genetic variations boost a person's own immune system to conquer tumors or at least keep them from spreading.
Razavi said it's only been in recent years that a convergence of two revolutions in science has enabled the pursuit of cancer detection that's truly early stage.
One revolution is the rise of DNA sequencing machines, particularly systems that can process huge volumes of data at increasingly fast speeds.
Illumina is the world's leader in this industry, and major scientists taking advance of this technology include genetics pioneer J. Craig Venter, whose institute sits across the street from the University of California, San Diego; cardiologist and customized-medicine evangelist Dr. Eric Topol of La Jolla, Calif., who works with the Scripps Health network and The Scripps Research Institute; and pediatric genomics expert Dr. Stephen Kingsmore of Rady Children's Hospital in San Diego.
The other revolution is an explosion of ever-more sophisticated supercomputers and software that help researchers make sense of the torrent of data coming from DNA sequencing systems. These data-analysis tools look for genetic patterns that indicate disease or protective benefits from among the hundreds, thousands and, conceivably one day, millions of patients' genomes that are studied.
GRAIL estimates that its extra-thorough process of cancer detection generates about 100 times more data - that's roughly 1 terabyte per patient - than traditional screening methods.
"There have been a lot of recent advances in sequencing technology and also in data computation that we just didn't have available just a few years ago," Razavi said.
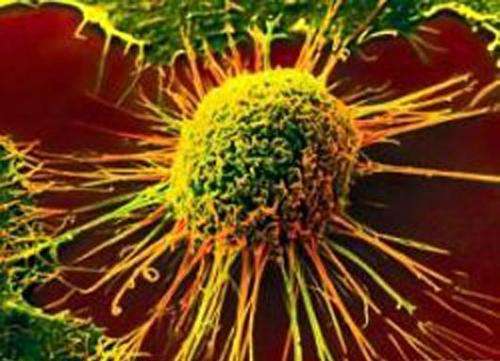
Often called "liquid biopsy" tests, these diagnostics capitalize on the fact that all cells shed bits of their DNA during their life cycles. And cells from cancer tumors are no different.
The problem is that the vast majority of "cell free" DNA floating in a person's bloodstream is not from cancerous tumors. In fact, researchers estimate that only 1 in 1,000 of these DNA snippets is from a cancerous cell, meaning that liquid biopsy tests have got to be very, very good at spotting the precise genetic mutations that signal cancer.
GRAIL is far from being the only business pursuing liquid biopsies. In fact, several companies' products are already on the market.
Currently, doctors can order biopsies designed to spot blood-borne DNA fragments from cancerous tumors, a process that can help them decide which targeted cancer drugs to use and can enable them to better monitor different stages of the disease. The tests can even let them know more quickly when cancer has returned after initial treatment.
But so far, going that extra step toward diagnosing cancer based on a blood test has remained on the horizon of possibilities.
The big difference between GRAIL's undertaking and others' efforts, Lichtenfeld said, is the company's commitment to conduct the huge clinical trials necessary to learn what it means when a mutated DNA fragment linked to cancer shows up in a patient's bloodstream.
Which fragments mean a patient will develop aggressive cancer and which don't? The only way to find out is to analyze the blood of thousands upon thousands of people who have or don't have cancer, then compare the results.
"It's not enough to find the cancer early. It's just as important to find out which cancer is going to be a problem and which is not. You only find that out by doing big trials that cost a lot of money," Lichtenfeld said.
Backed with more than $100 million in investments from the likes of Google, Bill Gates and Amazon's Jeff Bezos, GRAIL has the financial heft to mount an initial clinical trial of 10,000 patients - 7,000 who have been diagnosed with cancer and 3,000 who are cancer-free. A follow-up study for breast cancer aims to enroll 120,000 participants.
Lee, the head of clinical development at GRAIL, said the first clinical trial - the one with the 124 advanced cancer patients - was meant to build up a library of knowledge on how different cancers manifest themselves in the bloodstream. The idea was to better comprehend the lay of the land, if you will.
"We're trying to understand the full range of that kind of variability and all of the ways that cancer can manifest itself. More importantly, we want to understand how that cancer landscape can be distinguished from the landscape of people who don't have cancer," Lee said.
Once that knowledge base is large enough, it can be put to use in the massive breast-cancer trial, with hopes of accurately predicting cancer incidence in women undergoing routine mammogram screenings.
The plan looks unique, Lichtenfeld said.
"That kind of scale, I'm not aware of anybody else who has made that level of commitment at this point," he added.
But he noted that simply detecting cancer earlier will not be enough. Early detection must be coupled with therapies that can take advantage of those early warnings.
"The real grail is making a difference in people's lives. Otherwise, we're going to have a bunch of people walking around who have been told they have cancer with nothing they can do about it," Lichtenfeld said.
©2017 The San Diego Union-Tribune
Distributed by Tribune Content Agency, LLC.

















