Experts have new advice on prostate cancer screening. Here's why they put it back on the table
In a shift that puts early detection of prostate cancer back on the agenda of middle-aged men and their doctors, a federal panel of experts is recommending that men ages 55 to 69 weigh the potential harms and benefits of prostate cancer screening and judge whether getting tested feels right to them.
A recommendation issued Tuesday by the U.S. Preventive Services Task Force judged the "net benefits" of screening these men for prostate cancer to be small. But the panel said the prostate-specific antigen, or PSA, test should be offered to them "based on professional judgment and patient preferences."
For men 70 and older, the task force stuck with an earlier recommendation against routine prostate cancer screening.
The new guidance for men in late middle age is an unusual reversal of advice the panel offered in 2012. At that time, the task force suggested that for most men at any age, getting screened for prostate cancer just wasn't worth the risks—including anxiety, infection, erectile dysfunction and incontinence—of the unnecessary treatment that too often came with it.
Since then, the ledger of risks and benefits has changed on both sides.
As large studies have followed men for longer periods of time, researchers have seen that the PSA test can save lives—at least a few more lives than earlier believed—when used to screen men in their late 50s and 60s.
In a European clinical trial, periodic testing was initially found to prevent seven deaths for every 10,000 men screened. But with four years of additional follow-up, researchers have discovered the number of lives saved per 10,000 men screened is closer to 13. And mathematical models suggest that number will likely rise further as the men in the trial get older.
The increase "is not a big number," said Dr. Alex H. Krist, vice chairman of the task force, an independent group that operates under the auspices of the federal Agency for Healthcare Research and Quality. But the new data gave his panel "a little bit more confidence that fewer men would die" when more were screened before age 70.
At the same time, the responses of both doctors and patients to a prostate cancer diagnosis have undergone a significant shift.
In 2012, 90 percent of men who had their diagnosis confirmed with a biopsy were quickly ushered into surgery or treated with radiation, despite growing evidence that many of these cancers would never become dangerous.
Now, no more than 60 percent of such men proceed directly to treatment. The rest begin a process of "active surveillance" in which surgery or radiation is used only if the cancer progresses.
Meanwhile, urologists are using genetic testing, more precisely targeted biopsy procedures and improved imaging techniques to identify the more aggressive prostate tumors that warrant quick action.
Despite efforts to improve prostate cancer treatment, surgery and radiation therapy still exacts a high toll on patients: two out of three men will experience long-term erectile dysfunction, and about 20 percent of those who undergo radical prostatectomy will experience urinary incontinence.
But as more men "watch and wait," fewer men are exposed to the negative effects of treatment that might never have been necessary in the first place.
"That has changed the math of risks and benefits for screening," said Dr. David Penson, who chairs the Department of Urologic Surgery at Vanderbilt University in Nashville and was not involved in the new task force recommendation. "Take that small benefit and then reduce the harms of screening, and suddenly, the equation looks quite different."
In the United States, a man's risk of being diagnosed with prostate cancer at some point in his life is 13 percent, but his risk of dying of the disease is just 2.5 percent. Without screening, many men would never even know they had the disease, which can grow slowly for years. One-third of men who died in their 70s of other causes were found to have had prostate cancer.
For men between 55 and 69, the evolution of both knowledge and medical practice have made the question of whether to get the PSA test a potentially complex judgment call.
"This is what's called a preference-sensitive decision," said Ruth Etzioni, a biostatistician at Seattle's Fred Hutchinson Cancer Research Center who crunched the numbers from two of the largest clinical trials on prostate cancer screening but was not directly involved in setting the new guidelines. "It means the benefits and harms of the decision are going to be different for different people. Screening might be a good decision for you, but your friend may come up with a different decision."
Race would likely be a factor in those deliberations: African American men are nearly twice as likely to die of prostate cancer as white men.
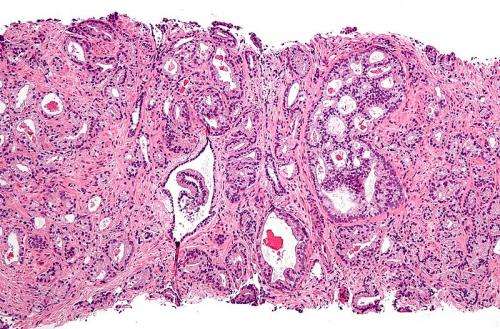
A family history of prostate cancer, and of cancers called adenocarcinomas (which include breast, ovarian, pancreatic and colorectal cancer), also might nudge a man toward regular screening. Smoking, too, is linked to a higher risk of death from prostate cancer.
The task force cautioned, however, that there is insufficient evidence on the role of race and family medical history to draft separate recommendations for subgroups.
"My typical prostate cancer consultation used to be 30 minutes," said Dr. Inderbir S. Gill, chairman of USC's Department of Urology. "Now it's become a one-hour, 15-minute consult, and we're not finished. That's the price of our evolving knowledge."
A man's decision should also take into account such intangibles as his tolerance for uncertainty and his willingness to act in response to an ambiguous threat to his health.
"Don't ask the question if you're not sure what you'll want to do with the result," said Dr. Christopher Saigal, the vice chair of urology at UCLA's Geffen School of Medicine who studies how doctors and patients make decisions about prostate cancer treatment.
Saigal, who was not involved in the task force's deliberations, said he remains convinced that for most men in the designated age group, PSA screening is a sensible choice.
"This is still the most common solid cancer in men, and it's treatable," he said.
But some men are skeptical of screening's value, and others are anxious that any possible threat to their health should be reckoned with head-on. Some have family histories of cancer, and others have so many health issues that a long-term threat like prostate cancer takes a back seat to more immediate concerns.
"The key thing is talking to the man before you draw his blood," Saigal said. Such nuanced discussions take time and time, and in modern medicine, time is in short supply. "We're moving into an era in which personalized medicine and shared decision making is going to come to the forefront. The data is too complex, and people are too complex, for one model to fit everyone."
The new task force recommendations are in line with those of the American Urological Association, which specify that men ages 55 to 69 with a life expectancy of more than 10 to 15 years be informed of screening's benefits and harms. The AUA notes that successive screening tests should be performed at least two years apart.
USC's Gill praised the new recommendations. But he added that the task force was not wrong in issuing its earlier, more skeptical views on prostate screening.
"This group very rightly said in 2008 and 2012, 'You urologists are hurting far more patients than you're helping, and the whole rigamarole starts when you take the PSA,'" Gil said.
"They have certainly stirred soul-searching in the urological community. They have certainly prodded urologists into acknowledging that yes, not every prostate cancer needs to be treated. They have done a great service."
©2018 Los Angeles Times
Distributed by Tribune Content Agency, LLC.















