A fungus usually found on skin might play a role in Crohn's disease
A fungus commonly found in human hair follicles also resides in the gut, where it may worsen intestinal disorders such as Inflammatory Bowel Disease (IBD) in patients with a certain genetic makeup, researchers report March 5 in the journal Cell Host & Microbe.
Malassezia yeasts found in oily skin and scalp follicles are linked to skin conditions, including dandruff. These microscopic fungi also end up in the gut, but it's not known how or what they do there.
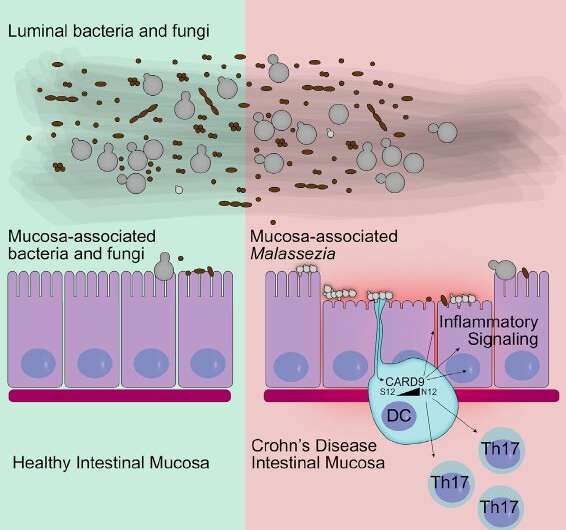
"We were surprised to find that Malassezia restrica was more common on intestinal tissue surfaces in Crohn's disease patients than in healthy people," says co-author David Underhill, Janis and William Wetsman Family Chair in Inflammatory Bowel Disease at Cedars-Sinai in Los Angeles. "Further, the presence of Malassezia was linked to a common variation in a gene known to be important for immunity to fungi—a genetic signature more common in patients with Crohn's disease than the healthy population."
IBD is characterized by changes in immune responses to the intestinal microbiome. While most studies on the microbiome focus on bacteria, Underhill's team investigates fungi's presence and its potential role in intestinal disease.
Changes in intestinal fungi such as M. restricta—and host responses to these fungi—may be a factor in exacerbating symptoms that contribute to disease in a subset of patients with Crohn's disease, says co-author Jose Limon, a Cedars-Sinai research team member.
The researchers had originally found that fungi are present in the gut microbiome of mice and that immunity against these fungi helps control gut-based inflammation. In mice, the presence of M. restricta worsened colitis, a type of intestinal inflammatory disease.
Looking at the mucosa-based intestinal fungi of healthy people and patients with Crohn's disease, a form of IBD, the researchers found several mucosa-associated fungi that were significantly more abundant in Crohn's patients. In particular, M. restricta was elevated in Crohn's patients carrying a genetic variation known as the IBD CARD9 risk allele.
This genetic variant enhances the ability of human immune cells to pump out inflammatory cytokines in response to M. restricta.
"The data so far do not suggest that the presence of Malassezia in the gut is an inherently bad thing. We found it in some healthy people, and in mice it does not seem to cause disease in the gut by itself," Underhill says. "However, if there is some intestinal inflammation, Malassezia seems to make it worse."
Next steps involve exploring whether eradicating this yeast from the intestinal microbiome in this subset of Crohn's patients alleviates their symptoms.
More information: Cell Host & Microbe, Limon et al.: "Malassezia Is Associated with Crohn's Disease and Exacerbates Colitis in Mouse Models" www.cell.com/cell-host-microbe … 1931-3128(19)30045-9 , DOI: 10.1016/j.chom.2019.01.007

















