Long-term care facilities serve as early indicators of community-wide COVID spread
A study led by researchers in the Arnold School's Department of Epidemiology and Biostatistics and the College of Arts and Sciences' Department of Psychology has investigated COVID-19 infection rates and deaths among long-term care facility residents and staff in South Carolina. Published in the Journal of the American Medical Directors Association (JAMDA), the team found that the early detection of COVID-19 in these settings could serve as a first indicator of disease spread in the surrounding area.
"COVID-19 has disproportionately impacted vulnerable populations, namely those over 60 years old, have pre-existing conditions, are overweight or obese, need assistance with daily activities, or have dementia or frailty," says Matthew Lohman, assistant professor of epidemiology and senior author on the paper. "Long-term care facilities tend to have more vulnerable populations, including older adults with pre-existing conditions; therefore, their residents are at greater risk of COVID-19 infection and adverse consequences, such as hospitalization and death."
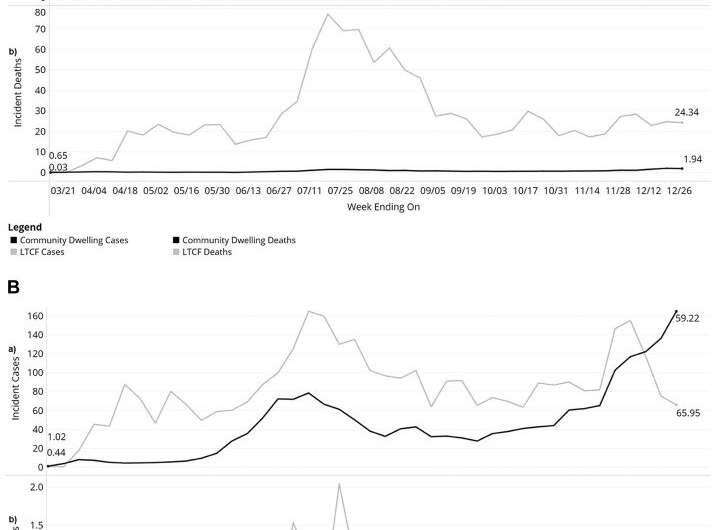
Through their analysis of data collected by the South Carolina Department of Health and Environmental Control's Infectious Disease and Outbreak Network, the authors found that long-term care residents experienced higher rates of infection throughout the study period (March 15, 2020 to January 2, 2021). Compared to older adults in the community, residents of these group facilities were also more likely to be hospitalized and 74 percent more likely to die.
Similarly, long-term care staff were more likely to contract COVID-19 than other community adults not employed in these settings. However, the two groups experienced similar death rates.
Within the 54,000 COVID-19 cases identified among older adults during the nine-month study period, 85.5 percent were in the community and 13.5 percent in long-term care facilities. Members of the latter group were more likely to be older, female, white and have pre-existing conditions. They were also more likely to be hospitalized (26.5 percent) than their counterparts living in the community (14.9 percent). Compared to the general population, long-term care staff were more likely to be female, black and have fewer chronic conditions.
The researchers point to pandemic response, particularly staff mitigation measures, at the state- and facility-level as significant factors impacting the spread of COVID-19 at long-term care facilities. Protective equipment availability, testing, and visitation policies at the facility-level, coupled with state and federal guidelines, can have positive and negative effects on residents' health (e.g., reduced vs accelerated spread) and quality of life (e.g., loneliness, anxiety, depression).
"The balance of resident well-being and safety is an important consideration when implementing control strategies," says Nicholas Resciniti, a recent graduate of the Ph.D. in Epidemiology program and lead author on the paper. "The disproportionate impact of COVID-19 on long-term care facilities highlights the need to understand and describe the spread of COVID-19 to help inform policies, preparedness, monitoring and coordination of future pandemic responses."
Over the course of the study period, the authors saw the gap between long-term care facility and community-wide infection and mortality rates narrow. This suggests that early detection of infections in these facilities could serve as a red flag to the greater community.
"Our results indicate that coordinated policies between long-term care facilities and the state/national level can facilitate early identification and rapid response to outbreaks to help stem the spread within the facilities and in the broader community," Lohman says. "For example, by having mitigation measures, such as masks and social distance policies, in place for different types of viruses and the ability to test individuals more quickly and frequently could help to identify cases early and yield better health outcomes."
More information: Nicholas V. Resciniti et al, COVID-19 Incidence and Mortality Among Long-Term Care Facility Residents and Staff in South Carolina, Journal of the American Medical Directors Association (2021). DOI: 10.1016/j.jamda.2021.08.006



















