Patients with stroke symptoms are evaluated safely for both stroke and trauma with new "STRAUMA activation"
A novel hospital alert called "STRAUMA" (a dual stroke alert and trauma activation) allows patients with stroke symptoms to be quickly assessed for traumatic injuries, without delaying the time to imaging of the brain and life-saving treatment. Research findings were presented at the virtual American College of Surgeons (ACS) Clinical Congress 2021.
Stroke is the fifth-leading cause of death in the U.S. Symptoms of stroke—weakness of one side of the body, dizziness and loss of balance, trouble seeing, and confusion—come on suddenly and can cause a fall or traumatic injury. An intravenous drug called tissue plasminogen activator (tPA) is used to dissolve the clot causing an ischemic stroke, the most common type. If a patient, however, is bleeding due to a serious injury, the drug may be harmful.
"The novel STRAUMA activation allows for an expedited evaluation of both stroke and trauma to facilitate timely administration of life-saving interventions," said lead study author Janet Lee, MD, a fourth-year surgical resident at UCHealth Memorial Hospital in Colorado Springs, Colorado. "Before administering tPA for the treatment of stroke, we want to rule out any injuries such as severe head trauma, intracranial hemorrhage, or bleeding risk that could cause catastrophic bleeding."
In 2018, researchers at UCHealth Memorial Hospital developed a dual alert protocol for both stroke and trauma. The protocol, "STRAUMA activation," enables the emergency department team and trauma team to assess the patient with stroke symptoms and signs of trauma first in order to identify a traumatic injury. If serious injury is not found, the patient can go for immediate computed tomography (CT) scanning to confirm stroke (ischemic or hemorrhagic, caused by a blood vessel rupture).
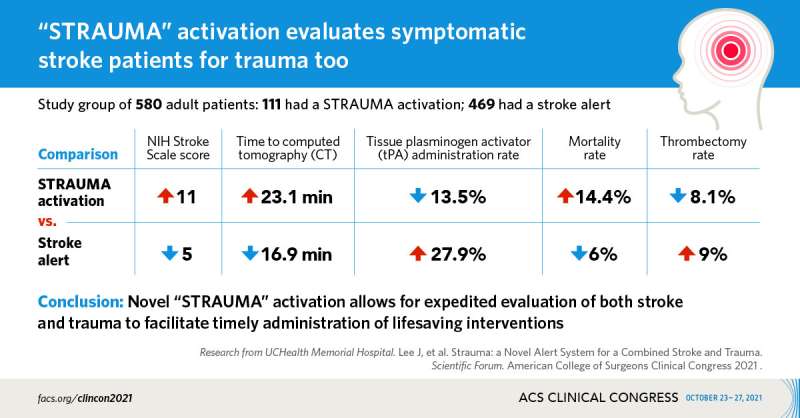
For this study, researchers sought to find out if issuing a STRAUMA activation, which adds an extra step to the process, has an impact on time-to-CT and time-to-tPA administration. They looked at the medical records of 580 adult men and women who had either a stroke alert or STRAUMA activation within 15 minutes of arrival at the level I trauma and comprehensive stroke center between January 2019 and September 2020. Of those, 111 had a STRAUMA activation and 469 had a stroke alert activated.
Key study findings include the following:
- The STRAUMA group had more neurological problems than the stroke alert group, scoring a median of 11 on the NIH Stroke Scale, compared with the stroke alert group who scored a median of 5. A score over 16 predicts death.
- The stroke alert group had a shorter time-to-CT than the STRAUMA activation group (17 minutes versus 23).
- The rate of tPA administration was higher in the stroke alert group than the STRAUMA group (27.9 percent vs. 13.5 percent). The reason is because there were fewer stroke diagnoses in the STRAUMA group.
- The rate of thrombectomy was similar between the STRAUMA and stroke alert group (8.1 percent vs. 9.0 percent).
- Overall, no differences were seen in time-to-tPA and time-to-thrombectomy in the stroke alert group and the STRAUMA group.
- The overall percentage of the STRAUMA patients who had a traumatic injury was 15 percent, with an average injury severity score (ISS) of nine. Severe trauma is defined as an ISS of 15 or higher.
- The STRAUMA group had a higher mortality rate than the stroke alert group (14.4 percent vs. 6 percent).
- After a multivariable analysis, NIH Stroke Scale and time-to-CT were predictors of mortality. The STRAUMA activation did not increase risk of mortality.
"The STRAUMA activation added six minutes to the overall process, whereas the stroke alert group had a shorter time-to-CT," Dr. Lee said. "It's all about risk versus benefit. The risk of patients with trauma getting tPA and having catastrophic bleeding outweighs the risk of a slight delay in CT scanning. And our results ultimately show that in all patients who did get tPA, no differences were seen in time-to-tPA."
The UCHealth trauma center gets about 80 STRAUMA activations each year. The authors are planning larger studies to compare clinical outcomes in stroke patients treated with the STRAUMA activation and the stroke alert protocols. Dr. Lee and colleagues will continue to monitor and refine the process to make it more responsive to patients.
"When we first started this activation system, we used signs of stroke and suspicion of trauma, but we found that approach resulted in a high over triage rate. That's why, in 2020, we changed the protocol to only include patients with external signs of trauma," Dr. Lee said. "We are continuing to accrue patients and monitor the outcomes that will help us further improve the process and patient outcomes."
More information: Lee JS, et al. Strauma Alert: a Novel Alert System for a Combined Stroke and Trauma. Scientific Forum Presentation. American College of Surgeons Clinical Congress 2021.



















