Estimation of R0 for the spread of SARS-CoV-2, a difficult key factor
In 2020, at the beginning of the pandemic, the whole of Germany was fascinated by the so-called R-value, which was published daily in the media. If it was above 1, it was clear that the pandemic would continue to spread. A value below 1, on the other hand, promised a decline in the number of infections. Values of more than 2, as calculated by the Robert Koch Institute during this time, did not bode well: they stood for an exponential spread of SARS-CoV-2.
However, a study now published in the journal Scientific Reports concludes that in reality, the R-value was significantly lower than previously assumed. Scientists from the Institute of Virology and Immunobiology and the Chair of Bioinformatics at the Julius-Maximilians-Universität Würzburg (JMU) are responsible for these calculations. Lead authors are virologist Carsten Scheller and bioinformatician Thomas Dandekar.
R0 value: Basis of many predictions
"The so-called basic replication number R0 of a virus describes the average number of people that an infected person infects in a population that has not yet had any contact with the virus," Carsten Scheller says.
Accordingly, R0 is a key factor when it comes to making predictions about the spread of a virus or to estimate how many people need to become infected to achieve the goal of herd immunity. "In addition, the R0 value can be used to predict whether a respiratory virus in temperate climates will develop more of a seasonal pattern of infection, such as influenza viruses, or whether there will be continuous transmission throughout the year," the virologist said.
Estimates vary widely
In the case of SARS-CoV-2, the R0 values determined varied significantly. An initial estimate based on data from 425 confirmed cases in Wuhan yielded a value of 2.26, while later calculations yielded 5.77. World Health Organization estimates ranged from 1.95 to 6.49, and the German Robert Koch Institute assumes an R value in the range of 2.8 to 3.89 based on systematic reviews.
"What all these estimates and calculations have in common is that they are based on the incidence of SARS-CoV-2 infections detected with a PCR test," says Carsten Scheller. The problem here is that these estimates depend not only on the characteristics of the population studied, but also on testing strategies and the increasing number of tests available and performed in the first weeks of the pandemic—at least if no mathematical corrections are made for this increase.
Excess mortality as a basis
To rid its calculations of such uncertain influencing factors, the team at the University of Würzburg decided to use a different data basis: the increase in mortality compared to pre-pandemic years, known as excess mortality.
"Since SARS-CoV-2 infection has led to increased excess mortality in many countries, these data can be used as a surrogate marker for the spread of coronavirus. And because excess mortality is independent of the number or strategy of tests performed, it provides a representative picture of the spread of infection in the general population," the virologist said.
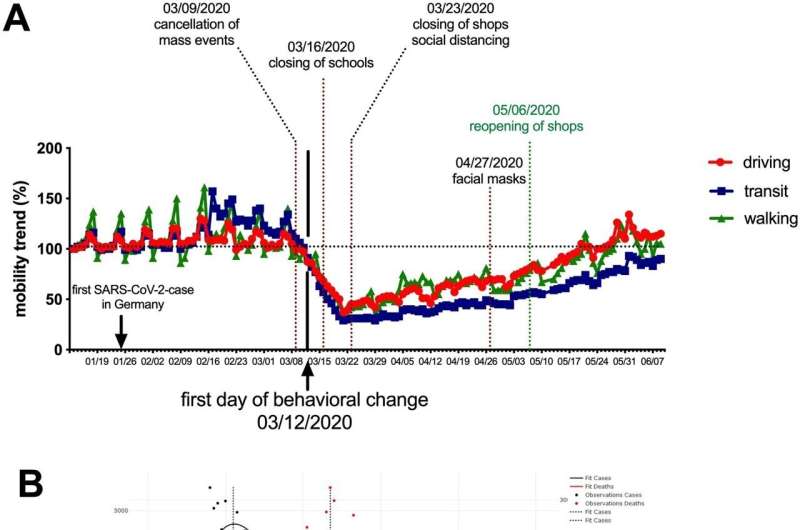
However, the team had to consider one important aspect: the question of the right time to collect the data. Germany, for example, had taken early measures to contain the SARS-CoV-2 epidemic—ranging from a ban on mass gatherings (March 9) to school closures (March 16) to a complete lockdown (March 23). All of these restrictions, as well as widespread media coverage, may have had an impact on the spread of the coronavirus, according to the researchers.
"For this reason, we used only deaths up to and including April 11, 2020, for our calculations. Since the infections of these deaths already occurred on average 25 days before death, the measures adopted to contain the infections could not have had any influence on the calculated value of R0," explains bioinformatician Thomas Dandekar.
Expansion of test capacities leads to overestimation
On this basis, the team concludes, "We determined an R0 value of 1.34 for infections in March 2020, which corresponds to a seasonal range of 1.68 in January and a minimum of 1.01 in July." This rather low range of R0 values is much more consistent with observations of pandemic progression than many earlier and much higher estimates, according to those involved in the study. The main reasons for this overestimation, they believe, is the massive expansion of testing capacity in the early stages of the pandemic, combined with changes in testing strategy.
This relatively low R0 value contributed significantly to a decline in infection numbers in the spring of 2020, according to the research group. The effects of the lockdown on the spread of the virus, therefore, may not have been as high as it might seem. Given a similar trend, therefore, any cost-benefit consideration of lockdown measures would have to be different than in the past.
New virus variants may have different R-values
What significance do these findings have now, given that other SARS-CoV-2 variants have long been sweeping the country? "The new, usually more contagious variants should certainly have a different R0 value in a human population unaffected by the virus than the original variant. However, this can never be calculated again, because the population has built up a great deal of immunity through infections it has already undergone and also through vaccinations," explains Carsten Scheller.
However, the lower R0 value of the original variant now provides a better view of the individual waves of infection. Finally, a low R value also means that herd immunity is achieved early on. Then the virus has no way to spread further, with the consequence that new variants are constantly being formed. "So the individual waves, caused by so-called immune-escape variants, are something quite normal," says the virologist. Once about a third of the population is infected, these waves of the original variant break off on their own, which is important to know for planning countermeasures, he says.
Limitations must be taken into account
However, the authors of the study now published are aware that their model is also subject to certain limitations. For example, pandemic-related medical shortages could lead to an increase in excess mortality that is independent of a direct effect of viral infections. Such a bias would lead to an overestimation of the R value.
In addition, statements about excess mortality always refer to a specific reference period, such as the previous year or, as in the case of this study, the preceding four years. Accordingly, an increase or decrease is always dependent on the development of mortality rates in the preceding years.
And finally, it is a prerequisite for the determination of correct values that the share of particularly vulnerable groups in the total infection incidence does not change significantly during the analysis period. Moreover, over time, the more infectious viral variants are preferentially passed on and eventually dominate the incidence of infection.
If all of these factors were taken into account, the authors of the study are convinced that excess mortality would be a valuable tool in future pandemics to determine reliable values for the rate of spread of an emerging pathogen in a population. Policy decisions could be better adapted to reality from this basis.
More information: Juan Pablo Prada et al, Estimation of R0 for the spread of SARS-CoV-2 in Germany from excess mortality, Scientific Reports (2022). DOI: 10.1038/s41598-022-22101-7


















