This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Pharmacists based in care homes found to be safer for residents
Basing specialist pharmacists in care homes can help make residents safer by cutting potential harm from medicines, according to research carried out by University of Leeds academics.
The Care Home Independent Pharmacist Prescriber Study (CHIPPS), which involved researchers in Leeds and across the country, trialed onsite pharmacists in dozens of care homes.
Evidence from the study shows that onsite pharmacists reduce the risk of potential harm to care home residents from medicines, cut down on unnecessary medicines, and ease the burden for GPs.
David Alldred, Professor of Medicines Use and Safety in the the University's School of Healthcare, led the project in Yorkshire.
He said, "Older people living in care homes have complex health needs and are usually prescribed multiple medicines. Our large-scale, high-quality study has shown that specially qualified prescribing pharmacists can safely prescribe for care home residents to ensure they are on the right combination of medicines."
"Importantly, the pharmacists also stopped medicines that were no longer needed or appropriate which reduces medicines burden for residents and is likely to prevent future side-effects. Key to success was the pharmacists building relationships and working in partnership with GPs, care home staff and residents."
According to the study, which was published in the BMJ, care home residents are routinely prescribed an average of eight or more medicines.
Medicine use is considered one of the main areas of risk in care homes by both the government and regulatory organizations.
One study cited in the BMJ paper says that 70% of care home residents experienced drug errors daily.
The University of Leicester-led study says that there have been regular calls for interventions to help to improve the management of medicine in care homes.
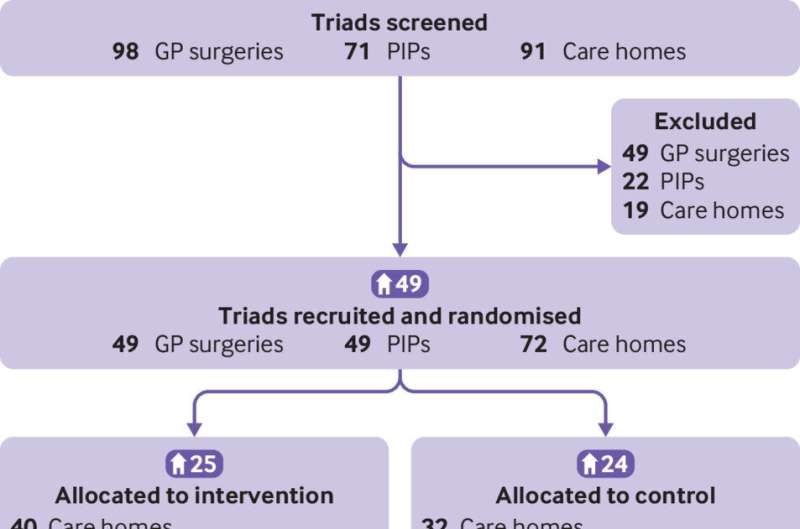
CHIPPS conducted a randomized controlled trial including 49 care homes across England, Scotland and Northern Ireland.
The study involved 25 care home trained pharmacist independent prescribers who were integrated into care homes to improve medicines management and safety.
It led to researchers determining that embedding pharmacist independent prescribers in care homes is safe, well received by all stakeholders and reduces potential future harm from medicines.
According to the study, independent monitoring of pharmacist activities and review of unexpected resident deaths and hospitalizations found no safety concerns.
Cutting unnecessary medicines
Interviews with general practitioners, care home managers, caregivers and residents showed they were highly satisfied with the service provided by the pharmacist independent prescribers.
Analysis of the primary outcome of falls did not show a significant reduction, but potential future harm from medicines was significantly reduced.
University of Aberdeen, Queen's University Belfast, University of East Anglia, NHS Norfolk Waveney and Norwich Clinical Trials also contributed to the research.
Project leader, Professor of Health Services Research and Head of School of Healthcare at Leicester, David Wright said, "I am delighted that the culmination of this six-year program of work, undertaken by an incredible group of researchers, clinicians and patient representatives has produced this result."
"The CHIPPS model of care was very well received by all stakeholders. We believe that this was because both our training and model of delivery focused on the integration of the pharmacist independent prescribers into the medical practice and care home teams."
"This approach was supported by our process evaluation, which found that the intervention appeared most effective when the pharmacists were embedded within their local general practice."
"Furthermore, our pharmacist-led intervention was reported by some GPs to reduce their workload as they no longer had to routinely review and authorize large numbers of repeat medicines and the pharmacist prescribers assumed some of their care home responsibilities."
"The results support expansion of the current pharmacist role in care homes, to include prescribing and frequent visits, as it reduces future harm from medicines and helps care homes to improve their management of medicines."
Professor Richard Holland who co-led the project, added, "Overall, this was a high-quality study which, through independent review of pharmacist care plans, hospitalizations and deaths, did not identify harm resulting from the pharmacist independent prescriber activities."
"This addressed concerns raised by some medical colleagues and a Scottish Ethics Committee at the start of the project, when we presented this model of care to them."
"Thus, this study provides important evidence for the development of models of care in care homes which we consider should include pharmacist independent prescribers."
More information: Richard Holland et al, Evaluation of effectiveness and safety of pharmacist independent prescribers in care homes: cluster randomised controlled trial, BMJ (2023). DOI: 10.1136/bmj-2022-071883





















