March 31, 2023 feature
This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
An antibody-based drug triggers rare inflammatory eye problems in macular degeneration patients
A drug approved in 2019 for macular degeneration apparently caused rare retinal side effects because of its interactions with the human immune system, two new studies have concluded.
The drug, a monoclonal antibody called brolucizumab, was developed by Swiss pharmaceutical giant Novartis AG for an eye condition known as wet age-related macular degeneration, or simply, AMD. The disorder is a leading cause of vision loss in people 65 and older. AMD not only causes severe blurring, it is characterized by a blind spot in the center of the retina, the macula of the eye. The disorder is characterized by an overgrowth of abnormal blood vessels that leak into the macula. Brolucizumab was developed to specifically target the damaging overgrowth.
The medication is approved in more than 70 countries, but while it was deemed safe in pre-approval testing, reports emerged a few months after its launch noting rare retinal disorders in a small percentage of patients treated with the drug. These side effects impacted an estimated 2.1% of patients, according to data in the journal Science Translational Medicine.
Scientists at two Novartis research centers embarked on investigations to determine what went awry. These probes were undertaken at the Novartis Institutes for Biomedical Research in Basel, Switzerland, and Cambridge, Massachusetts.
Scientists in one study examined serum samples, and in the other, created models of the inflammatory conditions patients experienced. The single aim of the research on two continents was to address the mystery underlying why this medication became linked to retinal side effects in some patients while the majority of patients treated with the drug were problem-free.
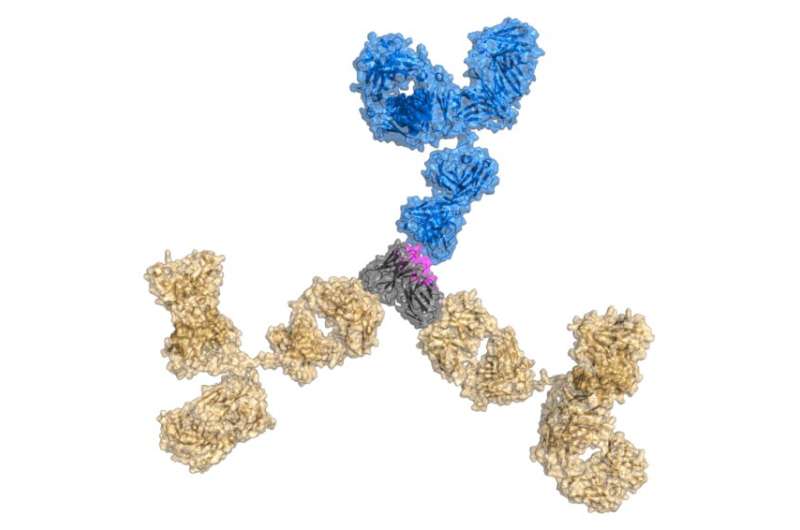
"In October 2019, Novartis launched brolucizumab, a single-chain variable fragment molecule targeting vascular endothelial growth factor A, for the treatment of neovascular age-related macular degeneration," wrote Anette C. Karle of the company's biomedical research division in Basel.
Vascular endothelial growth factor-A (VEGF-A) is a signaling protein with multiple activities, one of which is prompting the growth of aberrant blood vessels. Wet AMD is caused by abnormal blood vessels growing in the layer of the eye called the choroid, situated underneath the light-sensitive retina. Blood vessel overgrowth leads to vision loss in AMD.
Writing in the Science Translational Medicine, Karle noted that patients who didn't fare well on the drug developed telltale conditions of the eye. "In 2020, rare cases of retinal vasculitis and/or retinal vascular occlusion were reported, often during the first few months after treatment initiation, consistent with a possible immunologic pathobiology," Karle, lead author of one of the new studies noted.
Retinal vasculitis is an inflammatory condition affecting blood vessels of the retina, the light-sensitive tissue at the rear of the eye. The most insidious aspect of retinal vasculitis is the painless loss of vision. Retinal vascular occlusion, on the other hand, is caused by a blockage in veins moving blood away from the retina. The blockage can lead to edema—fluid retention—in the macula. This trapped fluid accumulates not only within the retina but under it, leading to rapid and severe loss of visual acuity.
According to the research by Karle and colleagues, retinal disorders were "inconsistent with preclinical studies in cynomolgus monkeys that demonstrated no drug-related intraocular inflammation, retinal vasculitis or retinal occlusion, despite the presence of preexisting and treatment-emergent antidrug antibodies in some [test] animals." However, a small number of patients in the clinical trial experienced the two inflammatory conditions after treatment with brolucizumab.
To understand why the medication didn't work for some patients, Karle and her collaborators compared serum samples from select groups: nonhuman primates, untreated healthy volunteers, and 28 patients from the clinical trials who experienced retinal vasculitis or retinal vascular occlusion after brolucizumab treatment.
Serum analyses revealed that an immune response against brolucizumab was a prerequisite for both side effects because only patients with retinal vasculitis or retinal vascular occlusion showed strong T cell responses to the treatment. Patients' immune systems were attacking their retinas after treatment with the drug.
In a second study, also reported in Science Translational Medicine, Dr. Jeffrey Kearns and colleagues adopted a translational approach to elucidate how the body can unleash inflammatory forces after treatment with brolucizumab.
Kearns' team, based in Cambridge, Massachusetts, and Basel, Switzerland, integrated structural modeling, immunological analysis, and other techniques to investigate the root causes of retinal vasculitis and retinal vascular occlusion.
"The presence of antidrug antibodies in these patients led to the initial hypothesis that immune complexes could be key mediators," wrote Kearns, a researcher at the Novartis Institutes for BioMedical Research in Cambridge, and lead author of the second study. "Although the formation of antidrug antibodies and immune complexes may be a prerequisite, other factors likely contribute to some patients having retinal vasculitis or retinal vascular occlusion, whereas the vast majority do not."
Kearns and his collaborators studied brolucizumab's effects in a systems pharmacology model that mimicked conditions in the eye. Using the model allowed researchers to identify several factors that drove the treatment's interactions with immune cells.
These factors included a linear epitope on the drug shared with gut bacterial proteins, and the appearance of non-native derivatives of brolucizumab after 13 weeks. These manifestations led to the formation of immune complexes between brolucizumab and anti-drug antibodies.
Karle and Kearns, along with their colleagues, caution that more work is needed for more definitive answers. Both researchers note that other unknown factors could be at play, as their experiments were limited by a dearth of intraocular clinical samples and a lack of genetic risk factors.
More information: Anette C. Karle et al, Anti-brolucizumab immune response as one prerequisite for rare retinal vasculitis/retinal vascular occlusion adverse events, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.abq5241
Jeffrey D. Kearns et al, A root cause analysis to identify the mechanistic drivers of immunogenicity against the anti-VEGF biotherapeutic brolucizumab, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.abq5068
© 2023 Science X Network




















