This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Diagnosing neurocysticercosis

The pork tapeworm (Taenia solium) can grow to be more than 20 feet long inside the human intestine, where it attaches to the intestinal wall using the 4 suckers on its scolex, which is only 1 millimeter in diameter. The scolex looks somewhat like a head, but the organism has no mouth or digestive tract and simply absorbs nutrients through its body covering.
Taeniasis occurs when a person consumes undercooked meat from a pig containing the organism in its cysticercal stage; upon entering the human intestine, the cysticercus matures into an adult tapeworm, where it can live for years. As unsettling as the idea of this creature living inside a human gut may be, the intestinal infection with T. solium (taeniasis) is usually fairly benign infection is typically asymptomatic and can be treated with a single dose of the antiparasitic drug praziquantel.
How the parasite enters the brain
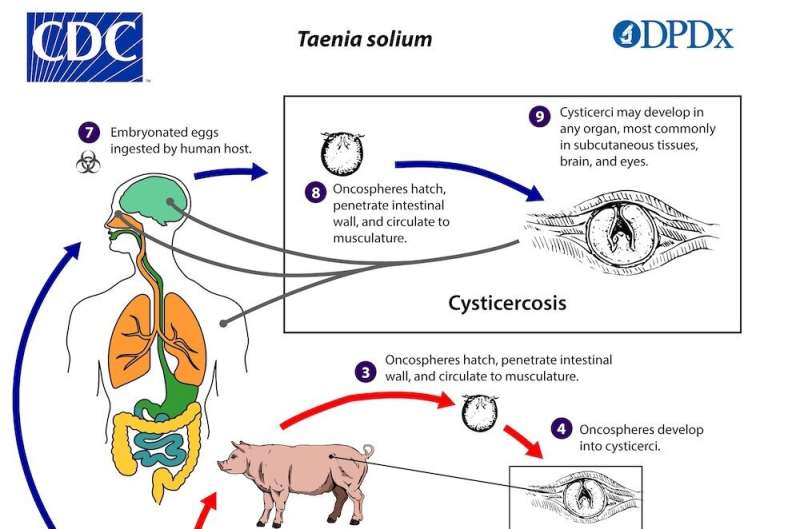
In contrast, if the eggs shed in the stool of an infected person are inadvertently ingested—either by the person with taeniasis or by people in their household or close environment—a much less benign disease process can result. (This "fecal-oral" route is a very common mode of transmission, employed by numerous pathogens, including norovirus). In the intestine, T. solium eggs hatch into oncospheres, which penetrate the intestinal wall and migrate through the blood to various tissues, most commonly muscle and central nervous system.
When cysts develop in the brain or other parts of the central nervous system, the condition is known as neurocysticercosis; between 2.5 and 8.5 million people worldwide are believed to have neurocysticercosis at present. In body tissues the larvae develop into cysticerci, just as they do in pig muscle. Because people, unlike pigs, are not (usually) consumed by other animals, the cysticerci do not have an opportunity to enter the digestive tract of another animal, where they would mature into adults, so humans are a dead-end host in this form of disease.
For months or years, cysticerci in the brain evade and even actively inhibit the host immune response, and people may be asymptomatic during this period, unless the location of the cyst causes symptoms (e.g., by blocking cerebrospinal fluid outflow, causing hydrocephalus). However, once the cysts begin to degrade, they elicit an immune response resulting in edema (swelling) and symptoms, including headache and seizures. In endemic areas, in fact, neurocysticercosis is responsible for 30% of cases of epilepsy.
Neurocysticercosis: The diagnosis
Neuroimaging findings in neurocysticercosis depend on the stage of the cyst. During the initial vesicular stage, in which the cysticerci are still viable, there is usually little swelling, but edema and inflammation surrounding the cysts become more prominent as the organisms are degraded and die. In the final stage, once cysts have been fully degraded, they become calcified.
A definitive diagnosis of neurocysticercosis can be made based on a single finding in only 3 scenarios:
- Observation of the scolex of a cysticercus (appearing as a "dot" in the center of the cyst) on neuroimaging.
- Visualization of a cysticercus behind the retina on ophthalmologic exam.
- Direct observation of a cysticercus on histopathology from a cyst that has been removed surgically, which usually takes place in cases where the cyst is located in the ventricles and causing obstruction of cerebrospinal fluid flow.
In many patients, however, none of these findings are present: scolices are often not apparent on imaging, retinal involvement is rare and the risks of a biopsy for diagnostic purposes alone are not usually justified. The diagnosis in these cases is less straightforward. Conditions other than neurocysticercosis (including bacterial abscesses, tuberculosis, toxoplasmosis, echinococcosis and non-infectious conditions such as tumor metastases) can cause cystic lesions in the brain that may be difficult to distinguish from neurocysticercosis.

Diagnosis in such cases must be made based on a collection of other supportive information. Clinical and epidemiologic data is often sufficient to make the diagnosis: for example, a person who resides in an endemic region, such as Latin America, India, China or sub-Saharan Africa, who presents with first-time seizures and is found to have multiple characteristic brain lesions, without evidence of any other type of infection, is extremely likely to have neurocysticercosis. By contrast, a person living with HIV, who has a low CD4 count, may be at risk of toxoplasmosis and intracranial tuberculosis, as well as neurocysticercosis.
People who live in non-endemic areas can also acquire neurocysticercosis, typically if they share a household with people who have intestinal tapeworm infection, or if they have spent time themselves living in an endemic area. But the diagnosis may be less obvious in these cases if there is not an initially apparent epidemiologic link.
In these ambiguous cases, antibody testing can be a helpful diagnostic tool. Enzyme-linked immunosorbent assays (ELISAs) are offered by several commercial reference laboratories, but these tests suffer from poor sensitivity, as well as cross-reactivity with other infections, most notably echinococcosis, another type of tapeworm infection. The gold-standard antibody test, which is performed by the CDC, is an enzyme-linked immunoelectrotransfer blot (EITB) assay. The assay was first developed in 1989, when improved treatments for neurocysticercosis (the antiparasitic drugs albendazole and praziquantel) had made the availability of an accurate diagnostic test more important for patient care.
The test was initially developed by sonicating 0.5 kg (more than a pound) of T. solium cysts, isolating the glycoproteins from this mixture and identifying a set of proteins to which serum and CSF from people with confirmed neurocysticercosis bound most effectively. This test has high sensitivity and specificity for neurocysticercosis, but because it requires submission of a sample to the CDC, the results can take some time to return, and sensitivity is lower in cases with only a single cyst or with calcified lesions. New tests for neurocysticercosis are in development, including antigen assays and PCR-based diagnostics; PCR is already used as a reference test method in Canada.
Treating Neurocysticercosis
Fortunately, the treatment for most forms of neurocysticercosis is relatively simple (usually consisting of a 10 to 14 day course of steroids and antiparasitic drugs), so people suspected of having the disease are often treated even in the absence of diagnostic certainty. The primary risk associated with treatment is seizure activity resulting from increased inflammation as the cysts begin to die during antiparasitic therapy. For this reason, people being treated for neurocysticercosis receive concurrent steroids and, in many cases, anti-epileptic drugs as well.
Ultimately, as with so many parasitic infections and other infectious diseases, no single test has perfect sensitivity and specificity for neurocysticercosis. Instead, the diagnosis relies on a combination of clinical, epidemiological, radiographic and serologic data and on input from clinicians, radiologists and clinical microbiologists.





















