This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
During the pandemic, hospital transfers were complex and distressing: Study examines decision-maker factors
During the COVID-19 pandemic, health care workers were frequently called upon to make decisions about whether to accept patient transfers from other hospitals, often due to a lack of beds, staff or the need for more specialized care.
These decisions would potentially prove to be the difference between life and death.
While existing guidelines for health care workers provide recommendations for how to allocate scarce resources in the hospital such as ventilators, recommendations for making decisions about transferring patients between hospitals were lacking.
A study from the University of Michigan Center for Bioethics & Social Sciences in Medicine examined the factors that went into this decision-making—and the moral distress that often resulted from it.
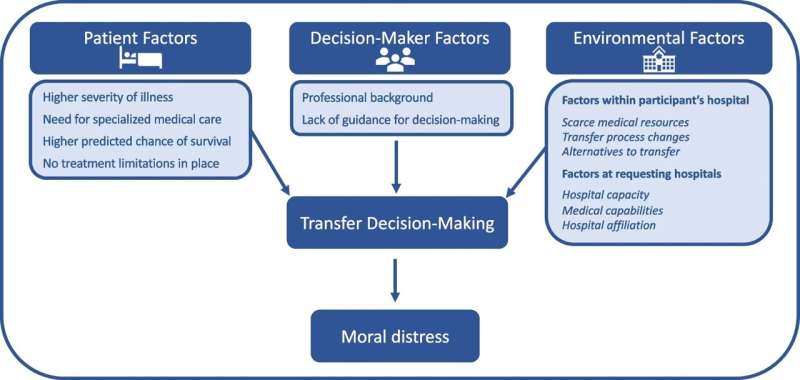
Via interviews with 21 physicians, nurses, and staff at hospitals across Michigan, the researchers, led by Emily Harlan, M.D., of the Division of Pulmonary and Critical Care Medicine and Andrew Shuman, M.D., of the Department of Otolaryngology in Head and Neck Surgery, identified three categories of factors that affected decisions to accept transfer patients: decision-maker, environmental and patient.
Decision-maker factors included the professional background of the person responsible for transfer choices. For example, physicians involved in transfer decisions were administrators who considered overall hospital capacity before deciding. Additionally, nurses were involved in triaging patients, information gathering and often responsible for discouraging family-initiated transfer requests.
Environmental factors included whether the receiving hospital was experiencing resource strain, for example, lacking space, staffing for beds, or equipment. Those interviewed revealed that many hospitals had to change their transfer processes, creating centralized transfer centers, or initiating remote support via telephone to create virtual intensive care units.
Finally, patient factors, such as severity of illness, the need for specialty care, and the likelihood of survival with escalated care played a significant role in decisions around who was transferred.
Close to 86% of those surveyed expressed moral distress, mostly related to denying patient transfers when there was no hospital capacity or to choosing which patient to accept from a long list of transfer requests. Moral distress is an important problem to address given the health care workforce is already facing high rates of burnout and staff shortages.
Given the impact on patients and clinicians, the authors suggest that guidelines be created to support decision-making about transfers and resource allocation, and that collaborative transfer teams be set up to potentially reduce the burden of decision-making and improve the patient transfer process.
The paper is published in the Journal of General Internal Medicine.
More information: Emily A. Harlan et al, Inter-hospital Transfer Decision-making During the COVID-19 Pandemic: a Qualitative Study, Journal of General Internal Medicine (2023). DOI: 10.1007/s11606-023-08237-w



















