This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Artificial neural networks can localize extra heartbeats, study shows
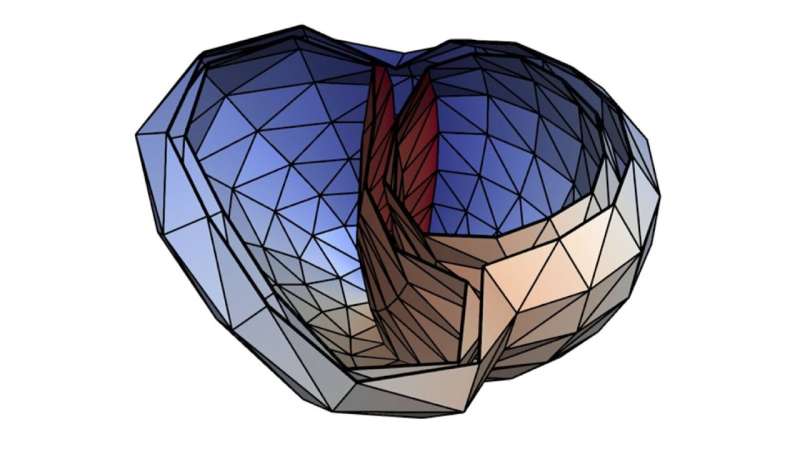
Additional heartbeats from cardiac chambers, so-called ventricular extrasystoles, may be associated with severe diseases. Researchers at Karlsruhe Institute of Technology (KIT) use machine learning for their non-invasive localization. This may facilitate and improve future diagnosis and therapy. The researchers used artificial neural networks trained with synthetic data from a realistic simulation model. They have reported their findings in Artificial Intelligence in Medicine.
Worldwide, cardiovascular diseases cause more than 17 million deaths per year. Of these, about 25% are deemed sudden cardiac deaths. They may be caused by ventricular tachycardias, i.e., quick cardiac dysrhythmias from the ventricles that are frequently caused by ventricular extrasystoles. These additional heartbeats from the heart chambers feel like skipped heartbeats.
Normal heartbeat is controlled by the sino-atrial node in the left atrium. Extrasystoles, by contrast, are caused by electrical signal sources at other places. Up to a certain number, ventricular extrasystoles are normal. Ventricular tachycardias, however, may impair cardiac action and even be life-threatening in case of existing cardiac insufficiency.
Ventricular tachycardias may be treated by catheter ablation: The origin of the extrasystoles is ablated by high-frequency current via a special catheter. For this, the origin must be localized precisely. Methods to insert a catheter into the ventricle for localization are minimally invasive but are time-consuming and are associated with certain risks.
Localization based on an electrocardiogram (ECG) requires prior acquisition of the patient-specific geometry with the help of tomographic imaging. "Machine learning methods, by contrast, enable identification of the origin of extrasystoles in a non-invasive manner and without tomographic imaging," says Dr. Axel Loewe, Head of the interdisciplinary Computational Cardiac Modeling Group at KIT's Institute of Biomedical Engineering (IBT).
Neural networks learn from 1.8 million ECGs
The researchers from IBT and from the company of EPIQure in Karlsruhe report how they use deep learning to localize ventricular extrasystoles from ECG signals without patient-specific geometries. For this purpose, the researchers use convolutional neural networks (CNNs). This is a special type of artificial neural networks, which is composed of various layers with different tasks. CNNs are suited for high data volumes and can be trained comparably quickly.
The researchers trained the CNNs with synthetic data obtained from a realistic simulation model exclusively. This was the only way to generate a data set of 1.8 million extrasystole ECGs. Finally, they evaluated their method using clinical data. In 82% of all clinical cases, the origin of the extrasystoles had been determined correctly. "Following further optimization using clinical data, our method will have the potential to accelerate medical interventions, reduce risks, and improve results," Loewe says.
More information: Nicolas Pilia et al, Non-invasive localization of the ventricular excitation origin without patient-specific geometries using deep learning, Artificial Intelligence in Medicine (2023). DOI: 10.1016/j.artmed.2023.102619





















