This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Take a deep breath: Early detection of vascular disease in chronic lung disease of premature infants
Premature infants often struggle with breathing and require ventilatory support and oxygen therapy. Unfortunately, this might lead to lung damage resulting in lifelong consequences and chronic disease.
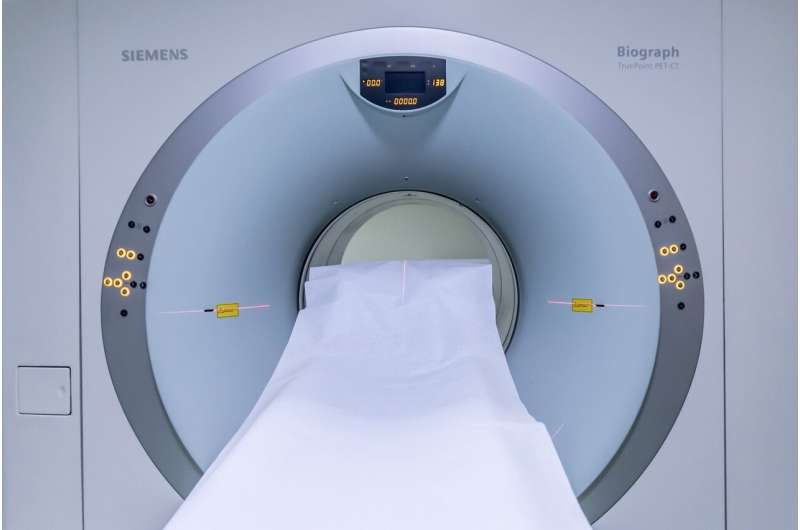
Dr. Anne Hilgendorff's team from Helmholtz Munich and the LMU University Hospital developed a non-invasive method with no need for sedation using MR imaging to detect early signs of vascular disease associated with chronic pulmonary impairment in premature infants, offering new avenues for risk stratification and potential prevention of complications later in life. The study is now published in the European Respiratory Journal.
Bronchopulmonary Dysplasia (BPD), a form of chronic lung disease affecting newborn infants, is the most prevalent long-term complication of prematurity. Premature infants may have difficulty breathing on their own. However, prolonged use of oxygen and medical ventilation can cause damage to their developing lungs, leading to BPD, which in turn, give rise to pulmonary vascular disease (PVD), a condition affecting the blood vessels.
This impacts the majority of infants struggling with BPD to differing degrees. PVD often goes unnoticed due to a lack of proper diagnostic tools for its early detection and is associated with a significant risk to develop pulmonary hypertension (PH) later in life. With this life-threatening complication, formerly premature infants represent a significant patient population in today's PH clinics.
The development of sensitive yet routinely applicable diagnostic tools for early detection would open up a window of opportunity for a whole new set of therapeutic opportunities and risk-adapted monitoring, thereby ameliorating or preventing the patients' lifelong struggles.
Physician scientist Dr. Anne Hilgendorff and her team from Helmholtz Munich and the LMU University Hospital along with LMU Radiologists and Neonatologists as well as scientists from Leiden University dedicated their new study to the identification and validation of early indicators of lung vascular pathology in newborns with lung disease.
New method to detect early signs of cardiovascular pathology in premature infants
In the new study, the team of researchers presents a method for the noninvasive detection of early signs of cardiovascular pathology in premature infants with BPD. Their new method makes use of a specific cardio-pulmonary magnetic resonance (MR) imaging protocol, meaning the scientists applied MR imaging to asses both the heart and the lungs of premature infants with and without BPD, who are close to their expected birthdate. Notably, the infants are not sedated during the procedure.
Altered blood flow from the heart to the lung through the pulmonary arterial (PA) together with signs of changes in cardiac function were recorded. From the resulting data, the team formed a statistical algorithm for the identification of signs of PVD. With this new tool risk stratification in formerly premature infants, known for their increased risk of sudden cardiac death in later life, can be improved.
For the first time, advanced MR imaging techniques were used in premature infants born before 32 weeks of gestation to demonstrate the synergistic power of changes in PA flow and cardiac function under consideration of prematurity at the time of BPD diagnosis to detect pulmonary vascular pathology.
The characteristic changes in PA blood flow and cardiac function were successfully linked to increasing pressure in the pulmonary circulation, likely stemming from a rarefied and remodeled vascular bed. In the very heterogeneous group of infants with milder BPD, the algorithm successfully identified those cases with a significant risk for PVD.
The non-invasive diagnostic strategy can be easily applied in clinics
The early detection of signs of PVD in premature infants with BPD using MRI harbors the possibility of categorizing premature infants into different risk levels for PVD and subsequent PH development and even sudden cardiac death in later life. The non-invasive nature of the newly presented diagnostic strategy and the potential to use highly standardized protocols in spontaneously sleeping infants makes this method suitable for clinical application.
Future studies will track the identified, early signs of lung vascular pathology into (pre)school age and adulthood to evaluate risk-adapted monitoring and treatment strategies in BPD.
More information: Friederike Häfner et al, MRI pulmonary artery flow detects lung vascular pathology in preterms with lung disease, European Respiratory Journal (2023). DOI: 10.1183/13993003.02445-2022 erj.ersjournals.com/content/ea … /13993003.02445-2022



















