This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Recovery checkups in primary care settings linked to increased substance use treatment and reduced drug abuse
Highly vulnerable patients with alcohol use disorder (AUD) or substance use disorder (SUD) who received regular assessments after their initial intervention had substantially better outcomes a year later than those who did not receive the same follow-up, according to a new study.
Fewer than one in ten people with SUD receive any form of treatment in a given year; among those who do, relapse and treatment reentry are common. A Screening, Brief Intervention, and Referral to Treatment (SBIRT) protocol is intended to facilitate treatment referrals, especially among patients with more severe SUDs, but research has shown it to be relatively ineffective in that regard.
Adding a Recovery Management Checkup (RMC) intervention can improve treatment rates; RMC conceptualizes AUD and SUD as chronic conditions requiring longer-term monitoring via regular check-ins, early re-intervention in cases of relapse, and treatment retention strategies.
For the study in Alcohol: Clinical & Experimental Research, investigators explored the impact of quarterly RMC checkups over 12 months on treatment and substance use among patients at Federally Qualified Health Centers (FQHCs), medical facilities serving populations experiencing socioeconomic hardship and often multiple chronic conditions.
Researchers worked with 266 participants in four FQHCs in Chicago, recruited between 2017 and 2020, who had moderate to high scores on an alcohol or drug screening test. Participants were predominantly male (65%) and African American (81%). In the past year, almost half had experienced homelessness, and fewer than half had been employed; most had problems related to physical and mental health and stress. All participants were referred for treatment.
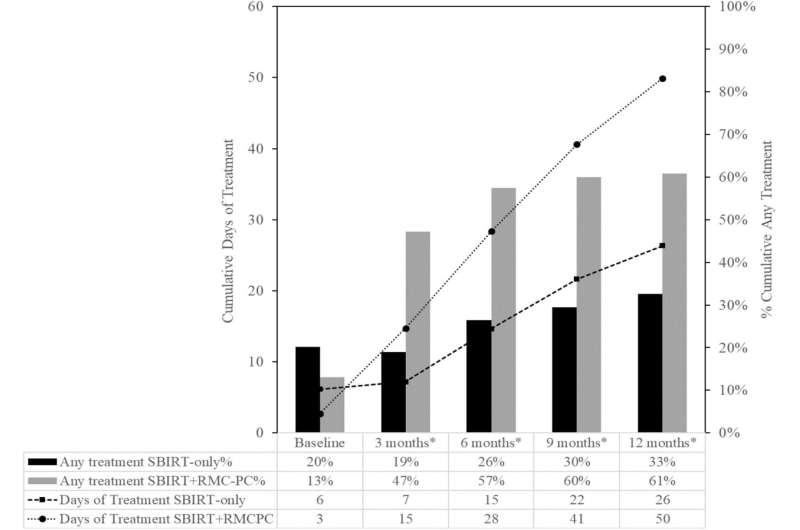
They were randomized to receive either SBIRT only or SBIRT followed by RMC. They were assessed at the start of the study and three, six, nine, and 12 months later. Those in the RMC group received personalized feedback and guidance using motivational interviewing and reinforcement of abstinence or support with reduced use and treatment.
Urine testing initially confirmed the broad accuracy of participants' reports, though it was discontinued during the COVID-19 pandemic. The investigators used statistical analysis to explore associations between the two intervention approaches and rates of treatment and substance use.
Quarterly checkups were associated with significant improvements in treatment initiation and reduced use of alcohol and cannabis, the most common substances. Over 12 months, participants assigned to SBIRT + RMC were more likely to attend treatment (61%) and received more days of treatment (mean 54 days) than those receiving SBIRT only (33%; mean 27 days).
Those receiving RMC also reported, on average, more days of abstinence (173 compared to 140) and fewer days of alcohol and cannabis use, and had lower alcohol and drug use severity scores. More days of treatment was shown to be the mechanism for more days of abstinence. The use of opioids (e.g., heroin) and stimulants (e.g., cocaine) did not differ between the two groups, however.
The study confirmed the value of using RMC to improve patients' linkage to treatment following SBIRT at FHQCs and demonstrated the added value of three subsequent checkups over 12 months. Among high-need populations, repeated assessments and connections to treatment may be a necessary element of care. More research is needed on the cost-effectiveness of RMC, which populations benefit most, and the real-world sustainability and scalability of the intervention.
More information: Christy K. Scott et al, A randomized controlled trial of recovery management checkups for primary care patients: Twelve-month results, Alcohol: Clinical & Experimental Research (2023). DOI: 10.1111/acer.15172 onlinelibrary.wiley.com/doi/10.1111/acer.15172




















