This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Strengthening routine care in African hospitals significantly reduces HIV-linked meningitis deaths
A research project studying how best to implement "back to basics" clinical and laboratory care in public hospitals in three African countries has halved the number of deaths from HIV-linked meningitis. The results are reported in The Lancet HIV.
A joint European and African research partnership, the DREAMM project, worked with local health leaders and health care workers, empowering them to design and implement changes to routine care for patients with HIV-related central nervous system conditions: cryptococcal meningitis, tuberculous meningitis, bacterial meningitis and cerebral toxoplasmosis.
The DREAMM project aimed to ensure that all HIV patients with symptoms of meningitis or cerebral toxoplasmosis were diagnosed and treated rapidly and effectively.
Despite the roll-out of antiretroviral therapy, there are still over half a million HIV-related deaths annually in Africa, of which a third are caused by conditions like meningitis that attack the central nervous system. These conditions should be treatable, but lack of diagnosis, the correct drugs and training on how to use these safely mean that many are fatal.
Working collaboratively on the ground
The project consortium researchers worked with the local Ministries of Health and empowered local health leaders, including hospital staff, to put in place rapid diagnostic testing and to ensure that the WHO cryptococcal meningitis treatment guidelines for confirmed cases were followed. Diagnosis involved both bedside point-of-care tests carried out by clinical staff and more detailed laboratory tests.
The project was led by Dr. Angela Loyse, a global health expert based at St George's, University of London, and African health researchers. It involved public hospitals in Malawi, Tanzania and Cameroon.
"By performing diagnostic tests such as lumbar punctures, on admission, the hospitals could get a rapid diagnosis, and then start treatment while the patient was still in the emergency area. This meant that ward care could become more about monitoring than chasing diagnostics. We also had in-parallel lab testing for quality control and to determine diagnoses not immediately clear by the bedside," says Loyse, lead researcher and senior lecturer in infectious diseases at St George's, University of London.
'Communities of practice'
Local health care leaders provided training—with support from the St George's and Institut Pasteur teams—for both frontline health care workers and laboratory technicians. The team set up "communities of practice" in each hospital, so experience could be shared between staff and ongoing support provided from health care leaders. Virtual ward rounds enabled doctors to discuss difficult cases with a mentorship community of senior doctors, laboratory experts and researchers online.
Dr. Cecilia Kanyama, an expert on HIV-related conditions, led the project in Lilongwe, Malawi. She said, "It was really encouraging to see the local leadership so involved and keen to take this on, particularly around the point of care testing. We were just facilitating, but there was excellent involvement of local key players, nurses and clinicians. That is really important to make this kind of intervention sustainable."
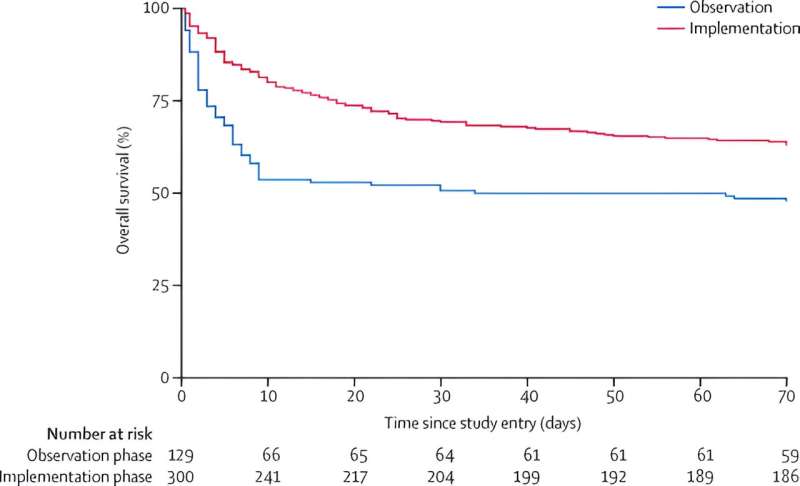
Before the training was provided and the new procedures put in place, the team followed the progress of patients presenting at the hospitals with symptoms of HIV-related meningitis, and found that within two weeks of admission to hospital, nearly half (49%) of these patients had died.
The new, co-designed procedures for dealing with HIV-related meningitis and cerebral toxoplasmosis were put into practice at each site for around 10 months, between January 2018 and March 2021.
Slashing deaths by half
The project recruited a total of 365 adults living with HIV who were admitted to hospital with a suspected first episode of CNS infection. Just under a quarter of these patients died (24%) within two weeks of admission, half the rate before the new procedures were put in place.
The researchers are now calling for the project to be urgently scaled up to reduce unnecessary deaths from HIV-related central nervous system infections. This is echoed by African health leaders on the ground.
Dr. Kanyama said, "Accessibility to point of care testing is really crucial and every hospital in Malawi should have it. Similarly with medication; tertiary level hospitals have it, but the district hospitals typically won't. We still have a very long way to go, but we've seen what is possible if these resources are made available."
"We've shown that optimizing the pathways for diagnosis and treatment of HIV-related central nervous system infections has a high potential to save lives, and that this is feasible in resource-limited settings. Access to essential tests and medicines in public facilities needs to be urgently ensured," says Loyse.
More information: Sayoki Mfinanga et al, Reduction in mortality from HIV-related CNS infections in routine care in Africa (DREAMM): a before-and-after, implementation study, The Lancet HIV (2023). DOI: 10.1016/S2352-3018(23)00182-0



















