This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Particular subgroup of antibodies responsible for dengue's increased deadliness may lead to vaccine
Dengue fever is a viral infection with a devastating twist: those who have caught it once are more likely to develop life-threatening disease the second time around. Why our bodies not only fail to learn from prior infection but also become more vulnerable as a result is a longstanding mystery that has prevented development of a universal dengue vaccine. Rather than protecting against disease, such a vaccine could instead serve as a first exposure to prime the body for it.
Now, new research has identified a particular subgroup of antibodies responsible for dengue's increased deadliness upon second exposure. The findings may open the door to more effective therapeutics—and at long last enable the development of a universal dengue vaccine.
"We definitively proved that it's not the presence of dengue antibodies that are a problem, but the quality of those antibodies," says Stylianos Bournazos, a research associate professor in the laboratory of Jeffrey Ravetch, the Theresa and Eugene M. Lang Professor at Rockefeller. "Now that we know the pathway that these antibodies use, we can develop therapeutics against it."
Homing in on the cause
Up to 400 million new dengue infections occur each year. A primarily tropical disease also known as break-bone fever, dengue spreads via mosquitoes, and most people who contract the virus for the first time will experience mild symptoms. Upon reinfection, however, about 10 percent of patients contract fever accompanied by aches, nausea, and rashes, with a small fraction of these patients experiencing life-threatening complications.
The question is why. Previous studies already pointed the finger at the antibodies that form against the virus, as opposed to other vestiges of infection. One such that antibodies are to blame is that newborns who were never exposed are still more likely to get severe dengue if their mothers had at one point been exposed.
"Only antibodies transfer from mother to baby, so this is the most definitive evidence that it's not just prior immunity, but the presence of antibodies, that influences susceptibility to dengue disease," says Bournazos.
Antibodies can occasionally cause severe infection rather than prevent it. Early versions of the RSV and measles vaccines were known to occasionally generate antibodies that bound the viruses in question but failed to prevent infection. Instead, these antibodies were associated with increased susceptibility to disease. The phenomenon was dubbed antibody dependent enhancement (ADE), and researchers have long suspected that ADE is responsible for dengue's odd pattern of infection.
But Bournazos and Ravetch suspected ADE was not the whole story. Why were only 10 percent of patients with prior dengue exposure ending up with severe disease? And why even among symptomatic cases there is a very wide spectrum of disease severity? "We noticed in these cases that people who experienced more severe disease all had elevated levels for a particular variant of these antibodies," Bournazos says. "This was our first clue that it's not just about the antibodies, but the type of antibody."
Of nanobodies and antibodies
It took several years for the team to develop the technology necessary to test their theory. Only recently, with help from the laboratory of Charles Rice, were Bournazos and Ravetch able to test human antibodies with human receptors in engineered mouse models of dengue.
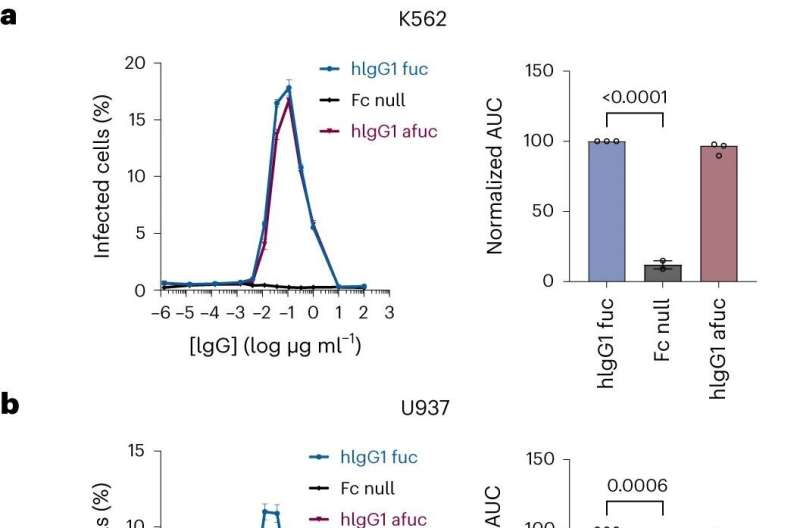
By not simply focusing on the antibodies but instead tracing the entire pathway of infection, the team demonstrated that severe outcomes weren't a product of the virus's ability to infect more cells (as one would expect were ADE to be responsible) but from the activation of a pathway leading to increased inflammation (a result that falls squarely on a problem antibody variant).
The findings upended the existing model of dengue infection, demonstrating that a small cadre of essentially "pathogenic" antibodies were primarily responsible for severe infection.
The team's results suggest that complications of severe disease could be prevented if patients were treated with a drug that disabled these pathogenic antibodies. On that front, the Ravetch lab has already developed nanobodies that target these pathogenic glycoforms well enough to prevent severe dengue in mice.
Similar nanobodies could one day be prescribed prophylactically to high-risk patients in the clinic. "The nanobodies would bring down the levels of pathogenic antibodies," Bournazos says. "That would go a long way towards preventing severe infections."
The study is published in the journal Nature Microbiology.
More information: Rachel Yamin et al, Human FcγRIIIa activation on splenic macrophages drives dengue pathogenesis in mice, Nature Microbiology (2023). DOI: 10.1038/s41564-023-01421-y



















