This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
More to learn about reducing the churn: Examining the pandemic's continuous enrollment Medicare policy
A new study led by researchers at the Harvard Pilgrim Health Care Institute has found that a federal policy implemented during the COVID-19 pandemic requiring continuous enrollment in Medicaid led to a significant reduction in the rates of becoming uninsured for adult Medicaid enrollees.
The study, "Continuous Medicaid coverage during the COVID-19 public health emergency reduced churning, but did not eliminate it," was published in Health Affairs Scholar.
Many people who have Medicaid coverage frequently gain and lose it, sometimes over short periods of time. This phenomenon is known as churning. Preserving insurance coverage in the wake of pandemic-related job loss was a priority in early 2020.
In response, the government implemented the Families First Coronavirus Response Act, a policy to protect rates of Medicaid coverage continuity. The policy required states to allow anyone validly enrolled by March 18, 2020, to remain on Medicaid for the duration of the public health emergency, despite almost any change in income or family circumstances that would otherwise make them ineligible.
"There is evidence that even short periods off of Medicaid have adverse consequences, like increased use of the Emergency Department, inability to take prescription medications regularly, and worse health," said Hao Yu, Harvard Medical School associate professor of population medicine at the Harvard Pilgrim Health Care Institute, and senior author of the study.
"A continuous enrollment policy like the one put in place during the pandemic is unprecedented; therefore, measuring its successes–and/or shortcomings–is important to reducing churning at the end of the public health emergency."
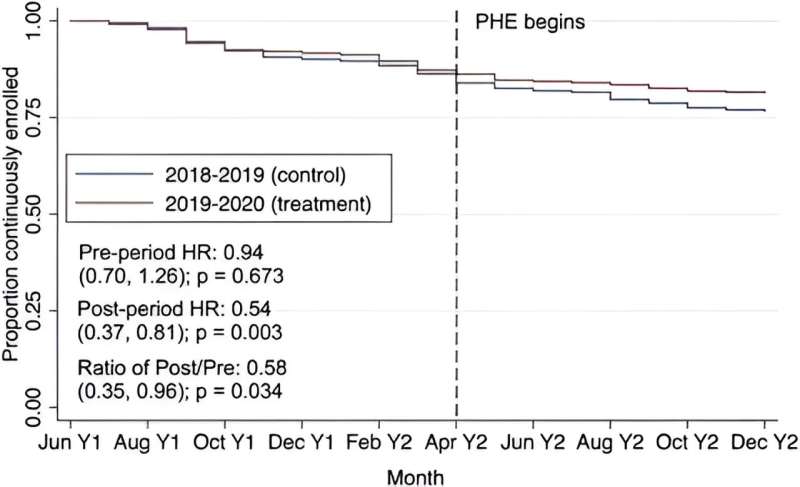
Using publicly available data from the Medical Expenditure Panel Survey—Household Component (MEPS-HC) from 2018—2020, the team evaluated nonelderly adults and children enrolled in Medicaid during 2019-2020 and compared them to their peers with Medicaid coverage during 2018-2019.
They found that, due to the continuous enrollment policy, rates of uninsured adults went down but were not entirely eliminated. These findings are early evidence that some of the Medicaid enrollment since the start of the pandemic and public health emergency can be attributed to reduced coverage loss and are consistent with existing evidence on the effect of the public health emergency continuous coverage policy, at least among adults. Rates of churning among children did not go down.
"Our work implies that over 300,000 people each month in the early pandemic avoided becoming uninsured as a result of the continuous enrollment policy and that a large part of the growth in Medicaid enrollment during the pandemic is a direct result of the policy," said Daniel Nelson, a research fellow at the Harvard Pilgrim Health Care Institute as part of the Harvard Medical School Fellowship in General Medicine and Primary Care and lead author of this study.
He added, "This is significant for policymakers to consider as they look to protect Medicaid enrollment at the end of the public health emergency."
More information: Daniel B Nelson et al, Continuous Medicaid coverage during the COVID-19 public health emergency reduced churning, but did not eliminate it, Health Affairs Scholar (2023). DOI: 10.1093/haschl/qxad055





















