This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
proofread
Team provides new insights into HIV prevention for cisgender women
Globally speaking, most HIV infections in young women occur in poorer countries, where up to 25% of women may be infected with the HIV virus. For heterosexual women, prevention through the use of Pre-Exposure Prophylaxis (PrEP) and its active ingredients, emtricitabine/tenofovir, represents one of the few options available to protect themselves from HIV infection. Additionally, it is a very inexpensive drug, available in most resource-constrained countries.
While pre-exposure prophylaxis (PrEP) is already being successfully used for homosexual men for several years, clinical studies have revealed an "extremely inconsistent picture regarding the putative efficacy of PrEP in women," according to von Kleist. The results of the clinical studies have subsequently generated uncertainty around the use of PrEP, which has had a direct impact on the corresponding WHO recommendations, as well as on the general acceptance and use of PrEP among women.
An international and interdisciplinary team, led by MATH+ Professor Max von Kleist (Freie Universität Berlin and Robert Koch Institute/RKI), has been researching this topic for 12 years. They have carried out an in-depth investigation of the allegedly different efficacy of the HIV pre-exposure prophylaxis (PrEP) in men and women. The scientists from the fields of medicine, public health, pharmacology, and mathematics have developed new modeling approaches and statistical tests based on the clinical data.
The paper is published in the journal Nature Medicine.
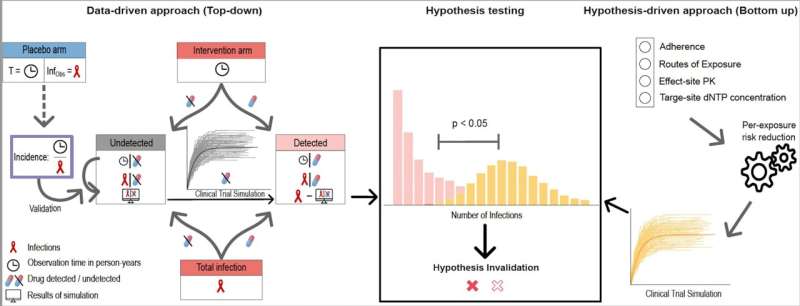
In contrast to a vaccination, clinical trial participants must actively take the PrEP medication themselves on a regular basis. The researchers found that some of the women in clinical trials did not actually take the medication at all and were, therefore, unable to achieve a protective effect. The researchers were initially able to "factor out" this proportion, as it would otherwise have falsified estimates of the biological effectiveness of PrEP. Then, they developed novel methods to estimate confidence intervals for the efficacy of PrEP in women based on the clinical data.
Confidence intervals indicate the range in which the actual value is likely to fall with high probability. Subsequently, in an independent mathematical modeling approach, they integrated all available data at that time to simulate hypotheses that were previously formulated to explain the putative difference in efficacy of PrEP between men and women. This dual approach made it possible to (in-)validate different hypotheses with statistical tests using the clinical data.
The study revealed that PrEP is indeed highly efficient in reducing the risk of HIV infection in women (>90%), and there is currently no indication that HIV protection with PrEP in heterosexual women should be less effective than in homosexual men. According to the study, the reasons for the supposedly differing effectiveness lie more in the PrEP-taking behavior and acceptance than in the biological efficacy in women. These results could mean a major change for cisgender women in terms of perception and the option of self-determined protection against HIV infection.
Based on this study, it is possible that the WHO may adjust its recommendations for PrEP use in women to align with those for men. Furthermore, mirroring the long-standing practice in homosexual men, further studies could also examine the effectiveness of using PrEP on demand for women.
Max von Kleist concluded by saying, "Since there is no solid evidence for a different efficacy of PrEP in men vs. women, it would therefore be logical to conduct research regarding the effectiveness of PrEP in women with 'on-demand' dosage, to create more options for HIV self-protection for women in the long term, and to bring about a greater decline in HIV in poorer regions."
More information: Lanxin Zhang et al, Model-based predictions of protective HIV pre-exposure prophylaxis adherence levels in cisgender women, Nature Medicine (2023). DOI: 10.1038/s41591-023-02615-x




















