This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Young people seeing GPs for mental health problems have low ongoing contact, finds study
Most children and adolescents in England presenting to their GPs with psychiatric symptoms have low or declining rates of ongoing contact, according to a study led by University of Manchester researchers.
The findings, published in The Lancet Psychiatry, could indicate that most children are in a low risk group and won't require long-term support, providing reassurance for children and their parents and caregivers.
However, the figures might also reflect an unmet need for some children and adolescents.
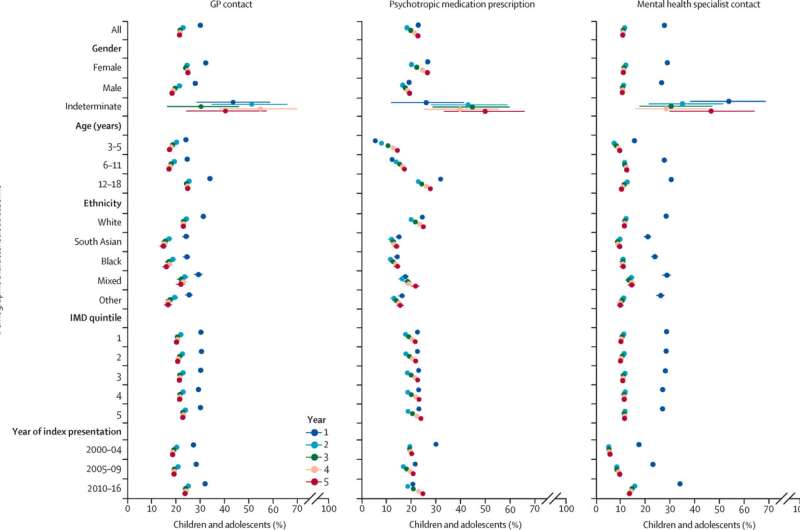
The study tracked the outcomes of around 370,000 3- to 18-year-olds over five years' using anonymized primary care health records from the Clinical Practice Research Datalink Aurum database.
All of the included children had symptoms of a possible psychiatric condition, such as depression, anxiety, Autism or ADHD. The research tracked the children's contact with health care services to find out what happened over the ensuing five years.
Almost 208,000 (51%) of the children and adolescents who presented with psychological symptoms to general practitioners had few subsequent health care contacts over the next five years and were very unlikely to be prescribed medications, or referred to specialist services for their mental health.
The largest of seven groups identified by the researchers, these children and adolescents also had the lowest risk of future hospitalization for either self-harm or suicide and were more likely to be younger, male, and from non-white ethnicities.
The next largest group (13% of the overall sample) had some ongoing contacts with the GP but didn't receive medications. The other groups identified had either declining rates of contact over five years, or prolonged high levels of contact with GPs or specialists, or escalating rates of contact. Each of these groups made up less than 10% of the overall sample.
Children and adolescents from Black, South Asian, and other non-white ethnicities had lower rates of ongoing GP contact and there were similar, less pronounced differences for mixed-ethnicity children and adolescents.
The findings are published as increasing numbers of children are seeking help for mental health symptoms, as well as ADHD and autism. The results provide some insight into what happens next for these children and suggests that for most of the young people, the problems they experience will be transient, or that they may receive the support they need outside of medical settings.
Lead author Dr. Morwenna Senior from The University of Manchester said, "Our findings show that a majority of children and adolescents with mental health symptoms have low or declining rates of ongoing contact with GPs and specialists.
"Increasing numbers of young people are experiencing mental health problems. At the same time, more children and families are seeking support from medical professionals for mental health conditions, ADHD and Autism.
"While this is concerning, previous research also suggests that for many young people, the prognosis is good and symptoms are likely to improve over time and this also fits with our findings.
"Though it's not clear if a proportion of this figure is because children are not receiving the medical support they need, this study can provide some reassurance to parents and children that many, if not most children will get better. It is also reassuring that the children in the low-contact group were the least likely to be hospitalized for self-harm, or to die by suicide."
Dr. Senior added, "Future research is needed to understand whether children and adolescents with low-contact trajectories have unmet needs, that we are not measuring, and whether they receive further help elsewhere. Linked datasets can be used to examine relationships between different groups of children and adolescents presenting with psychological symptoms, and their educational, social, as well as clinical outcomes.
She said, "We argue that services should differentiate between children and adolescents for whom early support might prevent deterioration from those whose symptoms are likely to resolve without further help.
"That could usefully inform changes to service configurations and preventive practice in services where resources are often stretched.
"For children whose problems are likely to resolve, reassurance and psychoeducation may be enough; whereas, for others, more intensive interventions might prevent deterioration in symptoms. We hope that our results will help distinguish these groups and better allocate limited resources."
Dr. Senior said, "These findings also add to substantial evidence that people's experiences and use of health care for psychiatric conditions in the U.K. varies according to ethnicity.
"However, in our sample, it is difficult to determine the reasons for these differences. It might be that there were differences in how helpful children and their families found the support they were offered; or there may be differences in how and where people access support. For example, support within education or from family networks could play a bigger role for Black and South Asian children and their families."
More information: Morwenna Senior et al, 5-year mental health outcomes for children and adolescents presenting with psychiatric symptoms to general practitioners in England: a retrospective cohort study, The Lancet Psychiatry (2024). DOI: 10.1016/S2215-0366(24)00038-5



















