This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Unraveling the link between the microbiome and esophageal cancer
Esophageal cancer (EC) is an aggressive malignancy with a poor prognosis, with its development and progression potentially influenced by changes in the esophageal microbiome. Recent studies have revealed that specific microbiome compositions might be linked to EC's development, response to treatment, and patient prognosis.
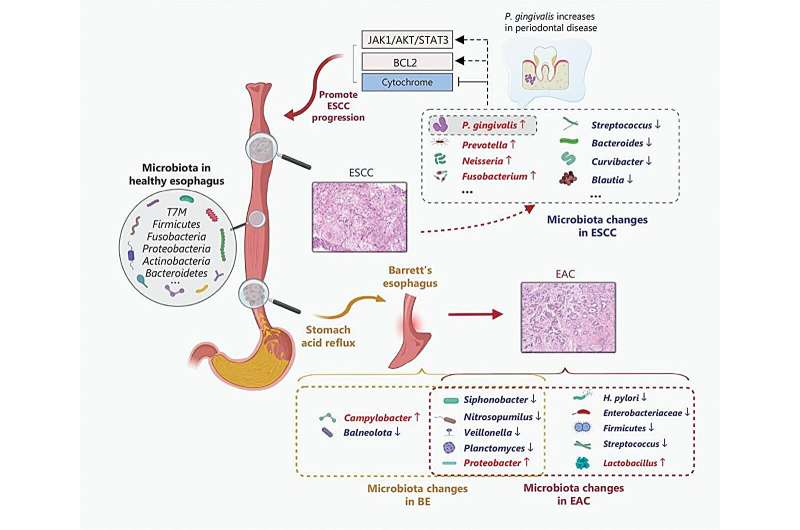
Esophageal cancer (EC) has two primary subtypes: esophageal squamous cell carcinoma (ESCC) and esophageal adenocarcinoma (EAC). These subtypes differ notably in geographical distribution, risk factors, and clinical characteristics. Despite considerable efforts, EC remains challenging to diagnose and treat due to its frequently late presentation and resistance to conventional therapies.
A comprehensive review, conducted by researchers at Zhengzhou University, Henan Cancer Hospital, and the Marshall Medical Research Center, marks a significant advancement in oncology. Published in the October 2023 issue of Cancer Biology & Medicine, the review highlights significant findings regarding microbiome changes in EC and their implications for disease pathogenesis and prognosis.
It identifies critical shifts in the microbiome associated with EC and explores how these changes might affect patient outcomes.
The researchers found that specific bacterial changes are linked to different stages of EC. For example, lactic acid-producing bacteria were more common in EAC, suggesting these microbes might support tumor survival by converting glucose into lactate, providing energy for malignant cells.
They also noted reduced microbial diversity in ESCC compared to non-tumor tissues. This decrease in diversity was associated with increased levels of Fusobacterium and decreased levels of Streptococcus, indicating that specific microbial profiles may play a role in cancer progression.
The study further explored how microbial dysbiosis might affect treatment outcomes. Distinct microbial compositions were associated with varied responses to radiotherapy and chemotherapy, emphasizing the potential of the esophageal microbiome to influence treatment efficacy.
"Understanding the role of the esophageal microbiome in the development and progression of EC could lead to earlier detection and more personalized treatment approaches," stated Dr. Hongle Li, one of the study's authors. "Our findings suggest that microbial dysbiosis may not only contribute to the pathogenesis of EC but also affect treatment outcomes."
The research has critical implications for early detection and improved treatment strategies for EC. Identifying microbial markers associated with disease progression could pave the way for targeted therapies that disrupt cancer-promoting bacteria. Moreover, specific microbial profiles could serve as prognostic indicators, aiding treatment planning and patient monitoring.
More information: Yi Li et al, Microbiome changes in esophageal cancer: implications for pathogenesis and prognosis, Cancer Biology & Medicine (2023). DOI: 10.20892/j.issn.2095-3941.2023.0177





















