This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Improving the conversion success rate of hepatocellular carcinoma
Hepatocellular carcinoma (HCC) presents significant challenges due to its high incidence and mortality rates, particularly in China where most patients are diagnosed at intermediate or advanced stages. This limits the applicability of curative surgical treatments to only 30% of cases, resulting in a five-year survival rate of 14.2%.
Recent advancements in locoregional and systemic therapies have introduced conversion therapy as a promising approach to downstage tumors in patients with initially unresectable HCC, potentially making them candidates for surgical resection and improving their long-term survival.
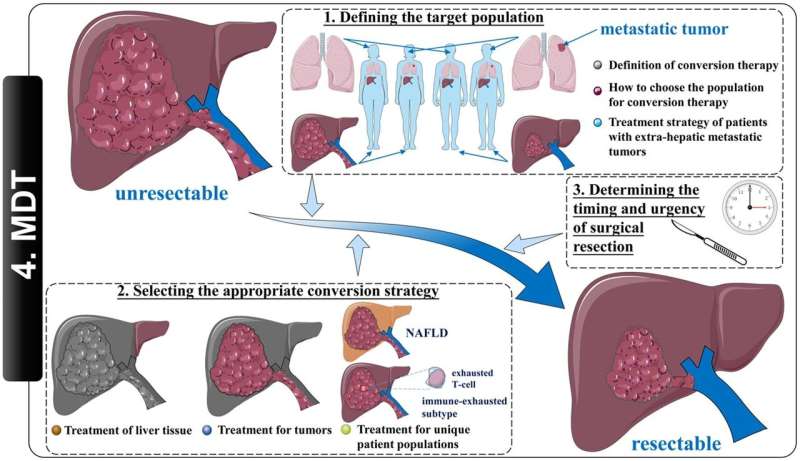
Conversion therapy aims to transform unresectable HCC into resectable lesions, enabling complete tumor removal. Identifying the right candidates for this therapy involves distinguishing between surgically and oncologically unresectable HCC.
Surgical unresectability is often due to inadequate future liver remnant (FLR) or the inability to achieve an R0 resection. Oncological unresectability refers to the inability to achieve optimal outcomes through surgery compared to non-surgical treatments.
Current guidelines, such as the "Guidelines for the Diagnosis and Treatment of Hepatocellular Carcinoma (2021 Edition)" and the "Liver Cancer Conversion Therapy Chinese Expert Consensus (2021 Edition)," suggest that patients in China liver cancer staging (CNLC) stage Ia-IIa and those with surgically or oncologically unresectable CNLC stage IIb and IIIa are potential candidates for conversion therapy. However, patients with diffuse infiltrative liver cancer or extensive bilateral lobar involvement face significant challenges in achieving successful conversion.
Conversion therapy strategies can be categorized into treatments targeting liver tissue and those targeting tumors. For liver tissue, procedures like portal vein embolization (PVE) and associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) aim to increase FLR. PVE is widely used with a conversion success rate of 60-80%, but it requires 4-6 weeks for FLR growth, during which patients may face risks of tumor progression. ALPPS offers a quicker FLR increase within two weeks and a higher conversion success rate (95-100%) but comes with higher perioperative complication rates.
For tumors, achieving a high objective response rate (ORR) while preserving liver function is critical. Monotherapies, whether targeted or immune-based, have limited ORR success, typically not exceeding 20%. Combination therapies, particularly systemic-systemic and systemic-local approaches, have shown to be more effective.
For instance, the "atezolizumab plus bevacizumab" regimen reached a 27.3% ORR in the IMbrave150 study, and the "lenvatinib plus pembrolizumab" combination achieved a 36% ORR in the Keynote524 study. These combinations help overcome resistance to tyrosine kinase inhibitors (TKIs) and immunological tolerance, enhancing the effectiveness of conversion therapy.
Several factors influence the success of conversion therapy, including patient selection, tumor characteristics, and the effectiveness of the conversion strategy. Key factors include:
- Patient selection: The careful selection of patients is critical. Ideal candidates are those with adequate liver function, absence of major vascular invasion, and good overall health. Patients with poor liver function or extensive disease involvement may not benefit as much from conversion therapy.
- Tumor characteristics: Tumor size, number, and location significantly impact the feasibility of conversion therapy. Smaller, localized tumors are more amenable to downstaging compared to larger, multifocal lesions.
- Conversion strategies: The choice of therapy, whether locoregional or systemic, affects the conversion success rate. Therapies that combine targeted treatments with immune checkpoint inhibitors have shown higher efficacy in reducing tumor burden.
Determining the appropriate timing for surgical resection post-conversion therapy is crucial. Patients should be continuously evaluated using the RECIST 1.1 criteria to assess their response to conversion therapy. Multidisciplinary team (MDT) evaluations are essential to devise individualized treatment plans and decide the optimal timing for surgery. This approach helps maximize the success rate of conversion therapy by ensuring that patients undergo surgery at the most opportune moment.
Adopting an MDT model is vital for the successful implementation of conversion therapy. This model involves collaboration among specialists from various fields, including surgery, oncology, radiology, and hepatology, to evaluate patients comprehensively and develop tailored treatment plans. MDT meetings facilitate the exchange of expertise and ensure that all aspects of a patient's condition are considered, leading to more effective decision-making and improved outcomes.
Conversion therapy holds significant potential for improving the prognosis of patients with initially unresectable HCC. By accurately defining the target population, selecting appropriate conversion strategies, determining the optimal timing for surgical resection, and promoting a multidisciplinary team model, the success rate of conversion therapy can be enhanced.
Continued advancements in treatment modalities and a deeper understanding of HCC are expected to further increase the efficacy of conversion therapy, ultimately prolonging the overall survival of HCC patients.
The research is published in the Journal of Clinical and Translational Hepatology.
More information: Qi-Feng Chen et al, Improving the Conversion Success Rate of Hepatocellular Carcinoma: Focus on the Use of Combination Therapy with a High Objective Response Rate, Journal of Clinical and Translational Hepatology (2024). DOI: 10.14218/JCTH.2023.00403


















